70 yrs old female with recurrent complicated UTIs .
August 8 - 2021
A 70 yr old female patient residing in Nalgonda is a homemaker presented to
OPD with
complaints of- loss of appetite since one week,
- generalised weakness since one week
- fever since 5 days
-burning micturation since 5days
History of present illness-
patient was apparently asymptomatic one week back then she gradually developed loss of appetite since one week which was not associated with nausea, vomiting, associated with generalised weakness
fever since 5 days which was high grade associated with chills and rigors, no diurnal variation, relived on taking medication, not associated with headache, cold , cough
she also started experiencing burning micturation since 5 days associated with low backache , no history of dark coloured urine or blood in urine
no h/o cold, cough, chest pain, palpitations, shortness of breath, pedal edema , reduction in urine output, diarrhoea, constipation, vomiting, nausea, pain abdomen
Past history:
she has been having similar episodes since 2016
she had 1st episode in 2016 it started with fever which was high grade associated with chills and rigors, associated with loss of appetite which were followed by loss of consciousness. she was immideatly rusged to a local hospital where the attenders were told that she had high blood pressure and had high blood sugars. she was diagnosed with UTI and was treated with parenteral antibiotics for 5 days and was discharged on oral antibiotics which she took for one week. since then she had been having recurrent episodes of UTI 2-3times every year. after the 2nd or 3rd episode she started having urinary incontinence for which she consulted a urologist and was said to have weakness of pelvic floor muscles and was advisced pelvic floor muscle strengthning exercises.
28 years back she underwent hystrectomy
25 years back she had complaints of generalised weakness
↓
went to a diagnostic center and got few investigations done
↓
consulted a physician and was diagnosed with type 2 diabetes mellitus and was started on OHAs
↓
she did not take OHAs regularly
during that time she was residing in Saudi Arabia and her husband took her to regular check ups almost every weekend during that period he sugars were under control with OHAs
↓
in 2007 they moved back to India in 2010 she had uncontrolled blood sugars for which she was started on insulin , she started using insulin pen
↓
in 2013 she consulted an endocrinologist and was started on injections Humalog (insulin Lispro) 28 units in the morning and Basalog ( insulin Glargine) 20 units at night
↓
started having tremors, weakness ,excessive sweating , and excessive hunger ( had recurrent hypoglycemic attacks) during which he son Dental surgeon adviced her to reducethe dose of Insulin lispro to 20 units
↓
reviewed with the same endocrinologist and was advisced to stop Insulin glargine and was told to take insulin lispro in the evening also
↓
had recurrent episodes of UTI and got hospitalised for the same
↓
10 years back she had chest pain for which she was taken to a cardiologist and was diagnosed with angina and was started on antiplatelets, statins and isisorbide dinitrate ( SOS) , tab febuxostat 40mg ( for joint pains), vitamin D3 supplementation, and was also advisced tab nitrofurantoin for 20 days since then she was on a regular follow up with the cardiologist every 3 months
she also started having complaints of tingling and numbness in her lower lower limbs and was diagnosed with peripheral neuropathy secondary to diabetes mellitus and was startedon tab. neuroprime plus ( alpha lipoic acid, thiamine, mecobalamine, elemental chromium)
was also diagnosed with CKD and anemia
↓
Diagnosed with Hypothyroidism 5 years back and was started on tab. levothyroxine 50 mcg daily before breakfast
↓
blood sugars were not under control in 2020 consulted an endocrinologist was started on sitagliptin 50mg and metformin 1000mg everyday morning before breakfast along with insulin
↓
in 2020 she was treated at home by her son for the similar episodes
↓
in 2021 march she had complaints of fever , cough and was diagnosed with COVID 19 infection and was hospitalized
there she was treated with Injection remdesivir for 5 days along with parenteral steroids and was later discharged on oral prednisolone and was gradually tapered over 10 days and then stopped
↓
in July she again had another episode of UTI and was again hospitalized
↓
was brought to our center
Personal history: married with 8 children - 4 sons and 4 daughters all are well at present,
no addictions - non smoker non alcoholic
sedentary habit
adequate sleep
no bowel abnormalities
family history- not significant
treatment history:
used insulin lispro (50%) + insulin lispro protamine 25 units in the morning and evening subcutaneously
used - Tab Ecospirin AV 75/10 mg H/S
tab Met -XL initially 25 mg for few years then 5o mg once daily
tab. feburic acid 40mg
tab tenegliptin 20mg then changed to tab sitaglipten 50mg + metformin 1000mg once daily
vitamin D3supplementation
used multiple antibiotics for recurrent UTI- nitrofurantoin, clarithromycin, piptaz, meropenem, levofloxacin
tab isosorbide dinitrate SOS
PROVISIONAL DIAGNOSIS:
A 70 years old lady with Recurrent complicated UTIs with peripheral neuropathy, secondary to diabetes mellitus (type 2) with hypertension with hypothyroidism known case of ischaemic heart disease.
GENERAL EXAMINATION:
patient is conscious, coherent, cooperative and oriented to time, place and person
patient is lying comfortably in supine position
patient is obese and well nourished
Height- 151 cms
Weight - 57 kgs
BMI - 25.0 kg/m2
face- wrinkled
eye- no abnormalities, baggy lower eyelids, pallor present, no xanthelasma or xanthomas
no cyanosis
oral cavity- lost all teeth, mucosa appears normal
nails- normal, no clubbing
no thyroid enlargement
no lymphadenopathy
neck veins- not distended
skin- normal, No pigmentation ,No scars, No atrophic changes
pulse- 110 beats per minute in supine position in right radial artery, regular rhythm, high volume, vessel is thickened, all other peripheral pulses are felt and are normal
BP: 110/80 mmHg in Right arm in supine position
100/80 mmHg in standing position
Respiration-- 20 breaths per min, thoraco-abdominal type
temperature- normal at the time of examination
feet-no pedal edema, no ulcers or calluses
GENITOURINARY SYSTEM EXAMINATION:
perabdomen- no abnormalities, no visible scars and sinuses
foleys catheter is insitu and is connected to urobag
no renal lump felt
renal angle- no tenderness
urinary bladder- empty
local examination - pubic hair-sparse distribution
labia majora, minora- atrophied
external uretheral meatus- no discharge, healthy
per vaginal examination bimanual examination
bilateral fornices free , non tender
anterior fossa normal
posterior fossa normal
Vault intact - no palpable masses felt, no tenderness
NERVOUS SYSTEM EXAMINATION
patient is conscious, cooperative, alert and oriented to time place and person
cranium and spine -normal, no abnormalities
speech- normal
Recent and remote memory intact
1. CRANIAL NERVES
CRANIAL NERVE | TEST | RIGHT | LEFT |
I | Sense of smell i) Coffee ii) Asafoetida | + + | + + |
II | i) Visual acuity – Snellens Chart ii) Field of vision – Confrontation test iii) Colour vision – Ishihara chart iv) Fundus | 6/6 Normal Normal Normal | 6/6 Normal Normal Normal |
III, IV, VI | i) Extra-ocular movements ii) Pupil – Size iii) Direct Light Reflex iv) Consensual Light Reflex v) Accommodation Reflex vi) Ptosis vii) Nystagmus viii) Horners syndrome | full 4mm Present Present Present Absent Absent No | full 4mm Present Present Present Absent Absent No |
V | i) Sensory -over face and buccal mucosa ii) Motor – masseter, temporalis, pterygoids iii) Reflex a. Corneal Reflex b. Conjunctival Reflex c. Jaw jerk | Normal Normal Present Present Present | Normal Normal Present Present Present |
VII | i) Motor – nasolabial fold hyeracusis occipitofrontalis orbicularis oculi orbicularis oris buccinator platysma ii) Sensory – Taste of anterior 2/3rds of tongue(salt/sweet) Sensation over tragus iii) Reflex – Corneal Conjunctival iv) Secretomotor – Moistness of the eyes/tongue and buccal mucosa | Present Absent Good Good Good Good Good Normal Normal Present Present Normal | Present Absent Good Good Good Good Good Normal Normal Present Present Normal |
VIII | i) Rinnes Test ii) Webers Test iii) Nystagmus | Positive Not lateralised Absent | Positive Absent |
IX, X | i) Uvula, Palatal arches, and movements ii) Gag reflex iii) Palatal reflex | Centrally placed and symmetrical
Present present |
|
X1 | i) trapezius ii) sternocleidomastoid | Good Good | Good Good |
XII | i) Tone ii) Wasting iii) Fibrillation iv) Tongue Protrusion to the midline and either side | Normal No No Normal | Normal No No Normal |
MOTOR SYSTEM :
Right. Left
Bulk: inspection UL normal normal
LL normal normal
palpation. UL Normal normal
LL normal normal
Tone: UL normal. Normal
LL. normal. normal
Power UL. 5/5. 5/5
LL: 5/5 5/5
Reflexes.
Superficial reflexes
Right. Left
Corneal. P P
Conjunctival P. P
Abdominal. + +
Plantar flexor flexor
Deep tendon reflexes
Right. Left
Biceps jerk. + +
Triceps jerk . + +
Supinator jerk. + +
Knee jerk + lost
Ankle jerk lost lost
SENSORY SYSTEM
RIGHT. LEFT
SPINOTHALAMIC
crude touch. UL lost in distal parts on both sides
LL lost in distal parts on both sides
pain. UL- lost in distal parts on both sides
LL- lost in distal parts on both sides
temperature. lost in distal parts on both sides in both limbs
post:
fine touch. lost in distal parts on both sides in both limbs
vibration. lost in distal parts on both sides in both limbs
position sensor. lost in distal parts on both sides in both limbs
cortical
2 point discrimination and tactile localization- could not be assessed
CEREBELLUM
titubation - absent
ataxia - absent
coordination- normal
no nystagmus
Romberg's sign could not be checked as patient was feeling weak
NO SIGNS OF MENINGEAL IRRITATION
AUTONOMIC FUNCTIONS:
positional tachycardia- absent
no orthostatic hypotension
sweating- normal
gait: could not be assessed as she was feeling weak
Investigations
FINAL DIAGNOSIS:
- Recurrent complicated urinary tract infections
- Complicated Fungal UTI
- Asymmetric Peripheral neuropathy secondary to Diabetes mellitus type 2
- Diabetic nephropathy
- known case of Ischaemic heart disease, Hypertension, Hypothyroidism
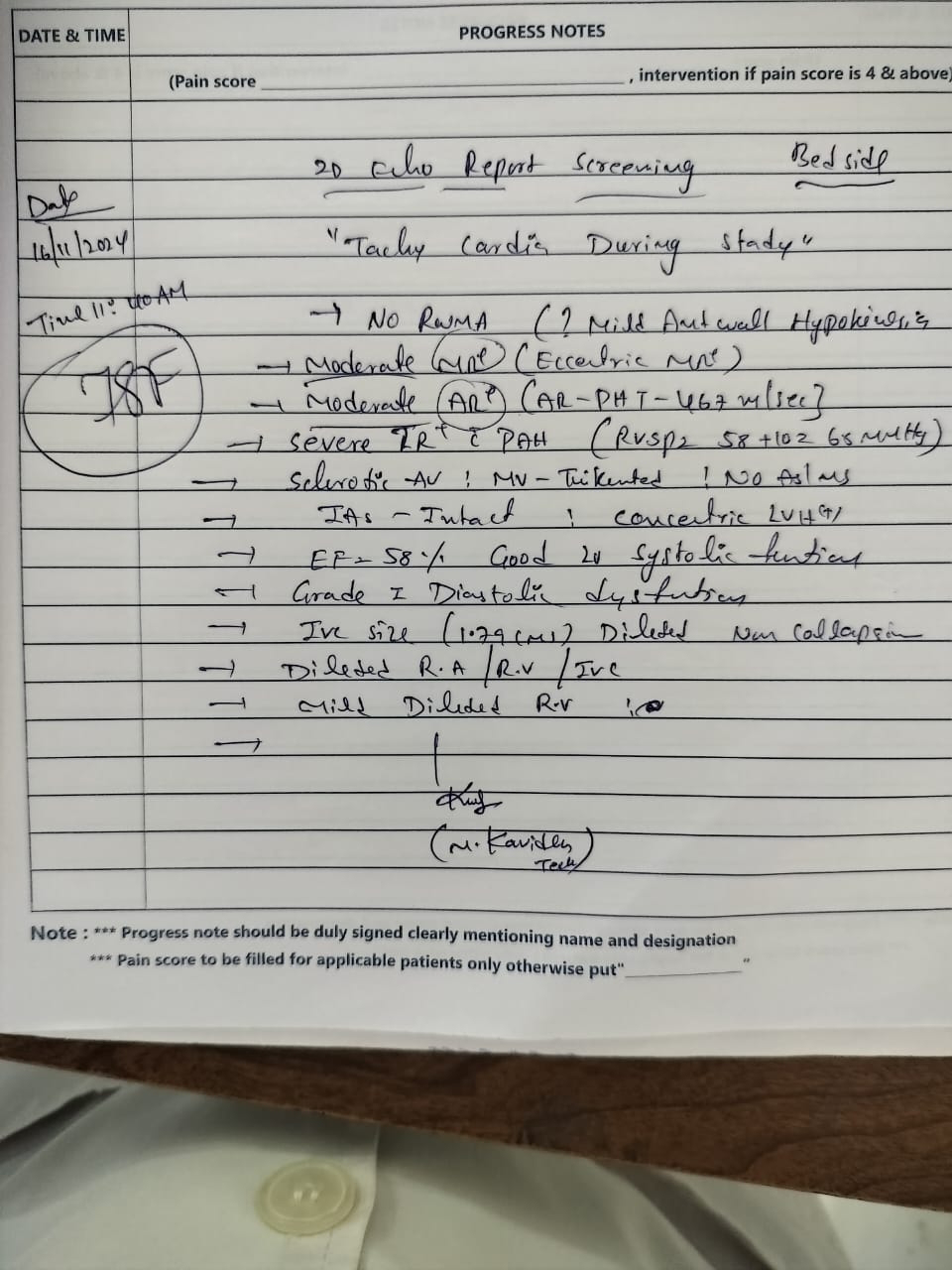
16-11-2024
PPM 1 - Readmitted yesterday to ICU again with LVF apparently but subjectively she appears to have become hard of hearing since lst admission and simply keeps complaining of inability to stand and walk due to extreme Fatigue!
Chest X-ray this afternoon.
Her paper based sketchy event timeline recorded this time. Can be compared with the other previous EMRs from all the previous admissions.
2D echo on paper. Now that our toy has been confiscated due to our being loud mouthed about it we have to contend with paper based imageology!@PPM2
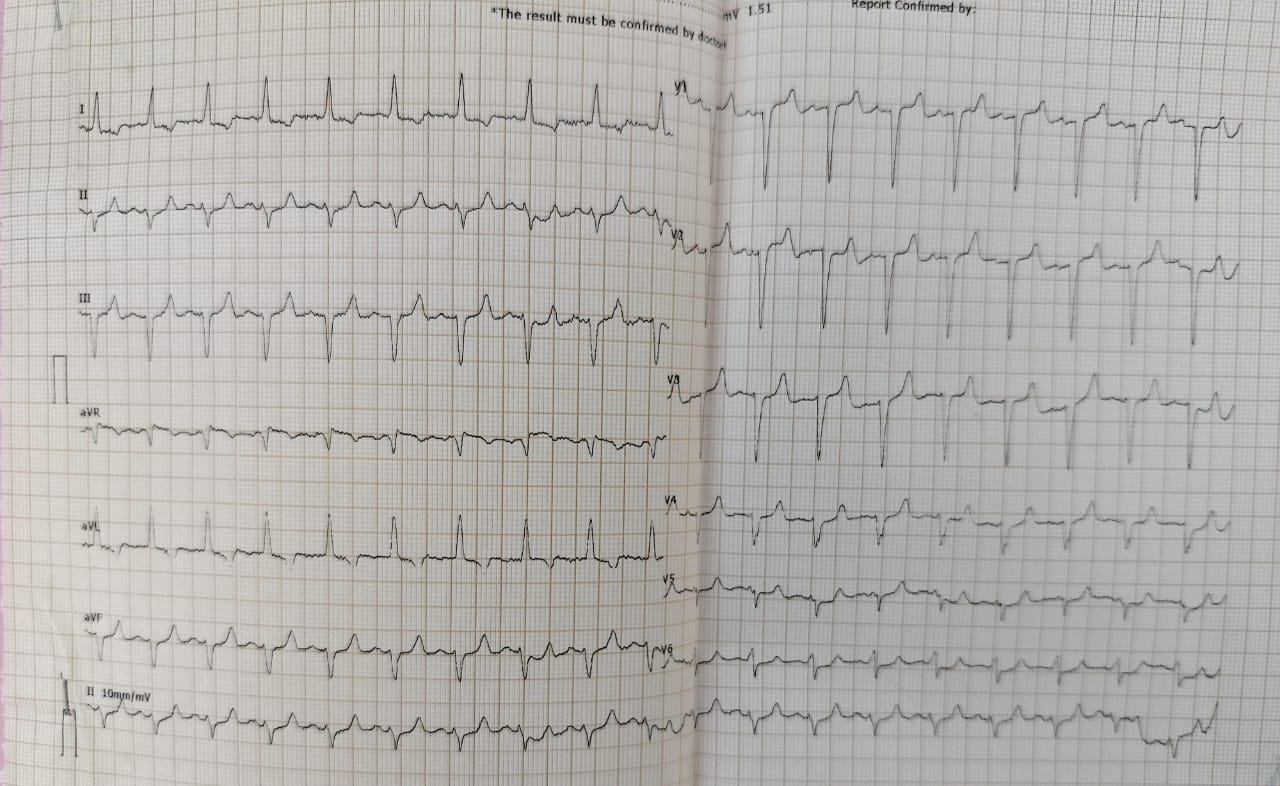
Tell tale ECG
PPM 2 - 👍
PPM 2 - What about being loud mouthed?
PPM 1 - It draws negative attention to one's work.
PPM 2 - And that can be quite discomforting!
PPM 1 - 👍
Age/Gender : 72 Years/Female
Address :
Discharge Type: Relieved
Admission Date: 07/02/2023 06:00 PM
Diagnosis
HHS WITH HEMIBALLISM,CHOREA-ATHETOSIS[MOVEMENTS RECOVERED AFTER 4 DAYS] LEFT SIDED UNILATERAL PULMONARY EDEMA [SECONDARY TO ACUTE CORONARY SYNDROME][RECOVERED IN 4 DAYS]
ANEMIA[? NUTRITIONAL CAUSE ?ANEMIA ]
CHRONIC UTI[MEROPENEM RESISTANT AND FOSFOMYCIN SENSITIVE E.COLI ] HYPOTHYROIDISM [15 YEARS,PRESENTLY ON TABLET THYRONORM 75MCG ] DIABETIC NEPHROPATHY[SERUM CREATININE-2.8 ON 10/2/2023]
K/C/O TYPE 2 DM[ SINCE 30YEARS]HBAIC-7% ON 8/2/2023 AND K/C/O HTN SINCE [SINCE 15 YEARS]
Case History and Clinical Findings
CHIEF COMPLAINTS-
GENERALISED WEAKNESS SINCE 1 WEEK COUGH SINCE 4 DAYS
INVOLUNTARY MOVEMENTS OF LT UPPER LIMB SINCE 1 DAY HOPI-
PT WAS APPARENTLY ASYMPTOMATIC 1 WEEK AGO THEN SHE DEVELOPED GENERALISED WEAKNESS
H/O COUGH SINCE 4 DAYS ,PRODUCTIVE, SCANTY SPUTUM -WHITE TO YELLOW IN COLOUR
,NON BLOOD STAINED ,NON FOUL SMELLING
H/O INVOLUNTARY MOVEMENTS OF LT UPPER LIMB SINCE 1 DAY [ TO AND FRO MOVEMENTS]
H/O INADEQUATELY CONTROLLED SUGARS FROM 4 MONTHS H/O FALL ONE WEEK AGO
NO H/O VOMITING ,SOB ,LOOSE STOOLS ,PAIN ABDOMEN,BURNING MICTURITION NO H/O FEVER,COLD,SORE THROAT
NO HISTORY OF SPEECH ABNORMALITIES
NO H/O WEAKNESS IN THE UPPER AND LOWER LIMB NO H/O LOSS OF CONSCIOUSNESS, MEMORY LOSS NO HISTORY OF ABNORMAL POSTURING
H/O FALL FROM BED AND COMPLAINTS OF PAIN IN THE HIP WHICH IS GRADUALLY RESOLVING
K/C/O TYPE 2 DIABETES MELLITUS SINCE 30 YRS ,ON INSULIN 10 YRS (INSULIN LISPRO 20 -X-20 )
K/C/O HTN SINCE 20 YRS ON T PROMOLET XL 50 MG PO/OD AT 10 AM AND T ATENOLOL 25 MG PO/OD
K/C/O HYPOTHYROIDISM SINCE 15 YRS ON THYRONORM 75 MCG
K/C/O RECURRENT URINARY TRACT INFECTION FOR WHICH SHE HOSPITALISED 1 YR BACK NOT A KNOWN CASE OF TUBERCULOSIS,EPILEPSY ,ASTHMA ,CEREBRO VASCULAR ACCIDENT ,CORONARY ARTERY DISEASE .
PERSONAL HISTORY:
DIET- MIXED APPETITE- LOST
BLADDER MOVEMENTS WERE REGULAR NON ALCOHOLIC ,CHEWS TOBACCO
CHEWS BETEL NUT AND BETEL LEAF TWICE DAILY NO ALLERGIES
FAMILY HISTORY-
NO H/O SIMILAR COMPLAINTS IN FAMILY
O/E OF PATIENT ON ADMISSION-
PT IS CONSCIOUS ,COHERENT, NON COOPERATIVE TEMP : 96.4 F
PR : 76 BPM
BP : 110/70 MM HG RR : 18/MIN
SPO2 98% AT ROOM AIR GRBS : 315 MG /DL PALLOR PRESENT
NO ICTERUS,CYANOSIS,CLUBBING,LYMPHADENOPATHY. BILATERAL PITTING TYPE EXTENDING UP TO KNEE
CVS : S1 S2 HEARD NO MURMURS
RS : BILATERAL AIR ENTRY+ NORMAL VESICULAR BREATH SOUNDS+ P/A : SOFT ,NON TENDER
BOWEL SOUNDS HEARD CNS-
MOTOR SYSTEM-
NORMAL TONE IN BOTH UPPER AND LOWER LIMBS POWER 5/5 IN ALL LIMBS
REFLEXES B / T / S / K / A / P
RT 1+ / 1+ / - / 1 + / - / F LT 1+ / 1 + / - / 1 + / - / F
SENSORY EXAMINATION NORMAL NO CEREBELLAR SIGNS
NORMAL GAIT AND NO MENINGEAL SIGNS GCS SCORE E4V5M6
O/E OF PATIENT ON DISCHARGE-
PT IS CONSIUOS ,COHERENT , COOPERATIVE
TEMP : 97.4 F PR : 76 BPM
BP : 130/60 MM HG RR : 18/MIN
SPO2 98% AT ROOM AIR GRBS : 191 MG /DL
CVS : S1 S2 HEARD, NO MURMURS
RS : BILATERAL AIR ENTRY+,NORMAL VESICULAR BREATH SOUNDS+ P/A : SOFT ,NON TENDER,BOWEL SOUNDS HEARD
CNS-
MOTOR SYSTEM NORMAL TONE IN BOTH UPPER AND LOWER LIMBS POWER 5/5 IN ALL LIMBS
REFLEXES B / T / S / K / A / P
RT 1+ / 1+ / - / 1 + / - / F LT 1+ / 1 + / - / 1 + / - / F
SENSORY EXAMINATION NORMAL NO CEREBELLAR SIGNS
NORMAL GAIT AND NO MENINGEAL SIGNS GCS SCORE- E4V5M6
COURSE IN HOSPITAL-
A 65 YR OLD FEMALE CAME TO THE THE CASUALTY WITH COMPLAINTS OF GENERALISED WEAKNESS SINCE 1 WEEK ,COUGH SINCE 4 DAYS AND INVOLUNTARY MOVEMENTS OF LT UPPER LIMB SINCE 1 DAY
H/O INADEQUATELY CONTROLLED SUGARS FROM 4 MONTHS
PT WAS EVALUATED WITH CLINICAL EXAMINATION AND AFTER NECESSARY INVESTIGATIONS, SHE WAS DIAGNOSED AS HYPERGLYCEMIA WITH CHOREA WITH DIABETIC NEPHROPATHY WITH RECURRENT URINARY TRACT INFECTION WITH IRON DEFICIENCY ANEMIA
AND FOLLOWING TREATMENT WAS GIVEN- NBM TILL FURTHER ORDERS
INJ HAI 6 U /IV/STAT AND FOLLOWED BY INSULIN INFUSION 1 ML/HR IVF NS @ 75 ML/HR
IVF 5D @ 50 ML/HR
GRBS AND VITALS MONITORING HOURLY
USG ABDOMEN AND PELVIS SHOWED BILATERAL GRADE 1 -2 RPD CHANGES WITH RAISED ECHOGENICITY
ECG SHOWED NORMAL SINUS RHYTHM
DAY 2
INVOLUNTARY MOVEMENTS OF LT UPPER LIMB NOT REDUCED
INSULIN INFUSION CHANGED TO SUBCUTANEOUS ROUTE, HAI AND NPH GIVEN ACCORDING TO GRBS
T PROMOLET XL 50 MG PO/OD AT 8 AM ,T THYRONORM 75 MCG PO/OD AT 7 AM ,T TETRABENAZINE 12.5 MG PO/OD AT 8 AM ADDED TO THE TREATMENT
T ATENOLOL WAS WITH HELD
OPHTHALMOLOGY OPINION WAS TAKEN IN VIEW OF ANY DIABETIC AND HYPERTENSIVE RETINOPATHY CHANGES
ON FUNDUS EXAMINATION NO CHANGES WERE NOTED IN RETINA . 2D ECHO WAS DONE SHOWED-
NO RWMA ,CONCENTRIC LVH + MILD MR+/AR+;TRIVIAL TR+ SCLEROTIC AV ,NOAS/MS
EF 58% ,RVSP=35 MMHG GOOD LV SYSTOLIC FUNCTION
DIASTOLIC DYSFUNCTION +,NO PE IVC SIZE (1.O7CMS) COLLAPSING
DAY 3
INVOLUNTARY MOVEMENTS WERE REDUCED COMPARED TO PREVIOUS DAY INJ NPH WAS WITH HELD
DERNATOLOGY OPINION WAS TAKEN IN VIEW OF DRY,BROWN SCALY LESIONS ON BOTH BOTH LEGS EXTENDING TILL KNEES
AND WAS DIAGNOSED AS SNILE XEROSIS AND ADVICED LIQUID PARAFFIN L/A BD FOR 4 WEEKS T TECZINE 5 MG SOS
BLOOD SENT FOR CULTURE SENSITIVITY SHOWED NO GROWTH NEUROLOGY OPINION WAS TAKEN AND ADVISED FOR MRI BRAIN
ANESTHESIOLOGIST OPINION WAS TAKEN FOR SEDATION FOR MRI
SO PAC WAS DONE I/V/O MRI UNDER SEDATION .PATIENT ATTEDERS WERE EXPLAINED ABOUT THE PROCEDURE AND POSSIBLE RISKS ASSOCIATED WITH MRI SEDATION
BUT PATIENT ATTENDERS REFUSED TO GIVE CONSENT AND MRI BRAIN WAS NOT DONE
DAY 4
INVOLUNTARY MOVEMENTS WERE REDUCED COMPARED TO PREVIOUS DAY
CULTURE AND SENSITIVITY OF URINE SAMPLE SHOWS ESCHERICHIA COLI >100000 CFU/ML OF URINE ISOLATED AND 5-6 PUS CELLS SEEN /HPF .
SENSITIVITY SEEN TO GENTAMICIN,FOSFOMYCIN,AND AMIKACIN INTERMIDIATE SENSITIVITY SEEN TO NITROFURANTOIN RESISTANT TO
AMOXYCLAV,CEFUROXIME,NORFLOX,COTRIMOXAZOLE,OFLAXACIN,CEFTAZIDINE,CEFEPIM
E,PIPERACILLIN/TAZOBACTAM.
DAY 5
SLIGHT INVOLUNTARY MOVEMENTS WERE NOTED INSULIN DOSE WAS FIXED ,HAI 8U----8U 8U
DAY 6
REDUCED INVOLUNTARY MOVEMENTS COMPARED TO PREVIOUS DAY
DAY 7
PATIENT IS SHIFTED TO ICU AT 12 AM IN VIEW OF FALLING SATURATIONS 60% AT ROOM AIR AND FEVER 100.7F
COMPLAINTS OF SHORTNESS OF BREATH
SHE WAS PUT ON INJ AUGEMENTIN 1.2 G IV BD
NEBULIZATION WITH BUDECORT AND MUCOMIST 8TH HOURLY INTERMITTENT CPAP
TAB NICARDIA 10MG PO/OD STAT GIVEN
PATIENT CONDITION HAS BEEN EXPLAINED TO THE ATTENDERS IN THEIR OWN UNDERSTANDABLE LANGUAGE ABOUT THE RISK ASSOCIATED WITH THE CONDITION AND IN NEW FALLING SATURATION AND POSSIBLE NEED FOR EMERGENCY INTUBATION
CHEST XRAY WAS DONE WHICH SHOWED LEFT SIDED OPACIFICATION[?CARDIOGENIC PULMONARY EDEMA ?PNEUMONIA]
DAY 8
INVOLUNTARY MOVEMENTS REDUCED COMPARED TO THE PREVIOUS DAY PATIENT COMPLAINS OF COUGH WITH EXPECTORATION
SPUTUM FOR AFB,GRAM STAIN AND ULTURE AND SENSITIVITY SEND
PULMO OPINION WAS TAKEN I/V/O HOSPITAL ACQUIRED PNEUMONIA AND ON EXAMINATION BILATERAL AIR ENTRY PRESENT
CREPS PRESENT AT INFRASCAPULAR REGION LEFT .RIGHT AND INTERSCAPULAR REGION AND LEFT IAA
THEY ADVISED CST,SYRUP ASCORIL LS 2TSP PO TID,NEBULIZATION WITH MUCOMIST BD,AND PLAN FOR BRONCHOSCOPY ONCE THE PATIENT IS STABLE
2D ECHO WAS DONE
RWMA PRESENT,LAD HYPOKINESIA,MILD LVH PRESENT [1.28CM]
MILD MR PRESENT,MODERATE TO SEVERE TR PRESENT WITH PAH,MODERATE AR PRESENT
SCLEROTIC AV NO AS/MS
EF 52% FAIR TO MILD LV DYSFUNCTION DIASTOLIC DYSFUNCTION PRESENT NO PE
IVC SIZE [1.64CM]DILATED COLLAPSING MILD DILATED RA/LA
DAY 9
NO FEVER SPIKES SINCE PREVIOUS DAY INVOLUNTARY MOVEMENTS ABSENT TAB TETRABENAZINE STOPPED
COUGH WITH EXPECTORATION REDUCED COMPARED TO THE PREVIOUS DAY INJ HAI S/C GIVEN TID 8 UNITS AT AM-1PM-8PM
SPUTUM FOR CULTURE SENSITIVITY -PSEUDOMONAS SPECIES IS ISOLATED SENSITIVE TO
PIPERACILLIN,GENTAMICIN,CIPROFLOXACIN,CEFTAZIDIME,AMIKACIN,CEFEPIME,TAZOBACT
EM,MEROPENEM
DAY 10
NO FEVER SPIKES SINCE PREVIOUS DAY INVOLUNTARY MOVEMENTS ABSENT
COUGH WITH EXPECTORATION REDUCED COMPARED TO THE PREVIOUS DAY
DAY 11
NO COMPLAINTS AND PT WAS DISCHARGED IN HEMODYNAMICALLY STABLE STATE
Investigation
2D ECHO WAS DONE SHOWED NO RWMA ,CONCENTRIC LVH + MILD MR+/AR+;TRIVIAL TR+ SCLEROTIC AV ,NOAS/MS
EF 58% ,RVSP=35 MMHG GOOD LV SYSTOLIC FUNCTION
DIASTOLIC DYSFUNCTION +,NO PE IVC SIZE (1.O7CMS) COLLAPSING
USG ABDOMEN WAS DONE SHOWED
BILATERAL GRADE 1 -2 RPD CHANGES WITH RAISED ECHOGENICITY
ECG SHOWS NORMAL SINUS RHYTHM
HBA1C 7%
HAEMOGRAM OF PT SHOWS HAEMOGRAM HB / TLC / RBC / PLT 7/2/23 7.9 / 13,100 / 4.34 / 2.50
8/2/23 8.4 / 11,000 / 4.55 / 2.99
11/2/23 8.0 / 13,700 / 4.31 / 2.74
SERUM OSMOLALITY 277.9
SPOT URINE PROTEIN 90.5
SPOT URINE CREAT 25.7SPOT URINE PROTEIN/CREATININE RATIO 3.52
CULTURE AND SENSITIVITY OF URINE SAMPLE SHOWS ESCHERICHIA COLI >100000 CFU/ML OF URINE ISOLATED
AND 5-6 PUS CELLS SEEN /HPF .
SENSITIVITY SEEN TO GENTAMICIN,FOSFOMYCIN,AND AMIKACIN INTERMIDIATE SENSITIVITY SEEN TO NITROFURANTOIN RESISTANT TO
AMOXYCLAV,CEFUROXIME,NORFLOX,COTRIMOXAZOLE,OFLAXACIN,CEFTAZIDINE,CEFEPIM
E,PIPERACILLIN/TAZOBACTAM.
URINE FOR KETONE BODIES WERE NEGATIVE
BLOOD SENT FOR CULTURE SENSITIVITY SHOWED NO GROWTH
SPUTUM FOR CULTURE SENSITIVITY -PSEUDOMONAS SPECIES IS ISOLATED
Treatment Given(Enter only Generic Name)
INJ HAI SUBCUTANEOUS 8U---8U---8U [8AM--1PM --8PM] IVF NS @ 75 ML/HR
INJ AUGMENTIN 1.2G IV/TID
T PROMOLET XL 50 MG PO/TWICE DAILY AT 8 AM 8PM
T THYRONORM 75 MCG PO/ONCE DAILY AT 8 AM
T TETRABENAZINE 12.5 MG PO/THRICE DAILY AT 8 AM -2PM-8PM LIQUID PARAFFIN L/A TWICE DAILY 8AM 8PM
T TECZINE 5 MG SOS
INJ LASIX 20MG IV/TWICE DAILY 8AM 4PM
SYRUP ASCORIL LS 10 ML PER ORAL THRICE DAILY GRBS 7.O PROFILE MONITORING
STRICT I/O CHARTING MONITOR VITALS
Advice at Discharge
INJ HAI SUBCUTANEOUS 6U----6U 6U[8AM-1PM-8PM]
TAB ECOSPIRIN -AV 75/20 PO ONCE DAILY AT 8PM
TAB HYDRALAZINE 12.5MG PO ONCE DAILY FOR 1 WEEK AT 8 AM
TAB LASIX 20MG PO/BD FOR ONE WEEK 8 AM 4PM
T PROMET-XL 25 MG PER ORAL TWICE DAILY AT 8 AM 8PM
T THYRONORM 75 MCG PER ORAL ONCE DAILY AT 8 AM
LIQUID PARAFFIN LOCAL APPLICATION TWICE DAILY [MORNING AND NIGHT] FOR 4 WEEKS SYRUP ASCORIL LS 10ML PO TID 8AM-----2PM 8PM
T TECZINE 5 MG PER ORAL SOS STRICT DIABETIC DIET
Follow Up
REVIEW AFTER 1 WEEK TO GENERAL MEDICINE OPD
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER
SIGNATURE OF PG/INTERNEE
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
Discharge Date Date:17/2/2023 Ward: AMC Unit:GM 2
https://pajrcasereporter.blogspot.com/2024/11/72f-diabetes-25yrs-mdr-uti-10yrs-honk.html?m=1
Age/Gender : 60 Years/Female
Address :
Discharge Type: Relieved
Admission Date: 15/08/2022 07:56 PM
Diagnosis
UNCONTROLLED TYPE 2 DIABETES MELLITUS WITH UNCOMPLICATED UTI (E COLI ISOLATED -FOSFOMYSIN SENSITIVE )WITH SYMMETRICAL PERIPHERAL DIABETIC NEUROPATHY WITH CHRONIC GLOMERULONEPHRITIS WITH CRF WITH CONGESTIVE CARDIAC Failure K/C/O ISCHEMIC HEART DISEASE ,HTN ,Hypothyroidism ,T2DM
Case History and Clinical Findings
PRESENTING COMPLAINTS:C/O Vomiting since 3 days.C/O Decreased appetite since 3 days.C/O Uncontrolled Sugars since 3 days.C/O SOB since yesterday night ( 14/08/2022)HOPI:A 72 year female presented to the casuality with complaints of low grade intermittent fever since 6 days which was relieved on taking medication. History of vomiting 2 episodes for 3 days which were non bilious and non projectile, food as content; associated with decreased appetite. History of SOB Grade III NYHA since yesterday night. No history of fever, cough, cold, chest pain, palpitations and burning micturition. Now admitted for further evaluation and management.PAST MEDICAL ILLNESS:In 1996, she sought for consultation for generalized weakness and was diagnosed with T2DM and started on OHA's; and started on Insulin therapy from 2010.In 2011, she had complaints of chest pain and sought for consultation and diagnosed with IHD; she was started on Antiplatelet, Statins, Febuxostat and Nitrofurantoin ( for 20 days) and adviced for regular cardiology follow up.In 2013, she had recurrent episodes of hypoglycemic attacks, sought for consultation for the same and her Insulin dosage was reduced.In 2016, She sought for consultation for fever, loss of appetite and LOC; admitted in hospital and diagnosed to be having UTI for which she was treated with IV Antibiotics and got discharged.Since then she was having Recurrent episodes of UTI 2-3 times a year.She then had symptoms of urinary incontinence, for which she sought for Urology consultation; diagnosed to be having Pelvic floor muscle weakness and adviced for pelvic floor strengthening exercises.In 2020, there is a slight pain in the knee joint and sought to a doctor and treated with a intra articular injection and there is increase in pain since then.In 2021,she had complaints of decreased urine output and burning micturation, swelling of both limbs and decreased appetite and vomiting and admitted in the hospital and given medication.Agust 2021 candidasep
tember 2021 klebsiellaMarch E.coli sensitive to carbapenems ,june sensitive to FosfomycinHistory of constipation since 3 years; since 2 years she was on regular medications for the same.SURGICAL HISTORY:S/P - Hysterectomy in 1993 under GA.COURSE IN YHE HOSPITAL:A 72 year female presented to the casuality with above mentioned complaints. Necessary investigations were done.
Chest xray showed cardiomegaly and 2D ECHO was done on 16/08/2022 which showed findings of:- Moderate MR/TR with PAH; Trivial AR; Mild Global Hypokinesia; No AS/MS; Sclerotic AV; Fair LV Systolic function; Eccentric TR; Diastolic dysfunction; No LV Clot; Dialated RA/LA and Concentric LVH; Minimal Pericardial effusion; IVC Size 1.93cms Dialated and non collapsing; EF 52%; RVSP 60mmHg.USG ABDOMEN was done which showed findings:1. Rt kidney 8.9×4.2cms; Lt kidney 9.8×5.5cms with normal size and echotexture; CMD maintained and Left PCS was dilated.E/O : Raised echogenecity of B/L kidneys with left hydroureteronephrosis.Her blood culture and sensitivity was negative and Urine c/s showed E coli growth, which was sensitive to fosfomycin.Surgical cross consultation was done i/v/o constipation and distended abdomen and orders followed.Urology cross consultation was done i/v/o left hydroureteronephrosis and adviced to get NCCT KUB to r/o ureteric stone.Nephrology cross consultation was done i/v/o raised creatinine and they priscribed to add supportive medications.Urine for ketones were negative; serum osmolality was 302; Serum Iron 46; serum LDH 180 IU/L; 24 hour urine creatinine 0.6g/day, protein 510mg/day, volume 1800ml; spot urine k+ 10.6, Na+ 180; Ncct kub was done on 19/08/2022 which showed:1. Soft tissue density at the left pelvi ureteric junction.2. Focal short segment thickening of distal part of left upper ureter.3. Left moderate hydroureteronephrosis.She was started on s/c insulin and her GRBS was with in normsallimits during the course in the hospital.Urology review cross consultation wa
s done after NCCT KUB, they advised to get CECT KUB, Cystoureteroscopy and Retrograde studies to rule out Transitional cell carcinoma. She was gradually improved and hemodynamically stable.
Treatment Given(Enter only Generic Name)
1) NORMAL SOFT DIABETIC DIET
2) IVF -NS /RL@75 ml/hr
3) INJ. HAI ACCORDING TO GRBS 8am-2pm-8pm 4)INJ. OPTINEURON 1amp IN 100 ml NS/OD 5)INJ.ZOFER 4mg I/OD
6)TAB. MET-XL 25mg PO/OD
Advice at Discharge
1. STRICT DIABETIC DIET
2. INJ. HUMAN ACTRAPID INSULIM 10U AT 8AM - 12U AT 2PM - 12 U AT 8 PM.
3. TAB. MET XL 25MG /PO / OD
4. TAB SHELCAL 500mg/PO/OD
5. SYP. BIO D3 /PO/ONCE WEEKLY
Follow Up
REVIEW SOS
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY (IF HAVING BURNING MICTURATION/ FEVER/ SOB/ CHEST PAIN ) CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER SIGNATURE OF PG/INTERNEE SIGNATURE OF ADMINISTRATOR SIGNATURE OF FACULTY
Discharge Date Date: 23/08/2022 Ward:GM
Unit:1
Second last admission:
Age/Gender : 70 Years/Female
Address :
Discharge Type: Relieved
Admission Date: 17/08/2024 12:13 AM
Diagnosis
ACUTE PULMONARY EDEMA SECONDARY TO LEFT VENTRICULAR FAILURE ( RESOLVED) HEART FAILURE WITH MID RANGE EJECTION FRACTION SECONDARY TO OLD CAD
IRON DEFICIENCY ANEMIA
K/C/O HYPOTHYROIDISM SINCE 15 YEARS K/C/O TYPE 2 DM SINCE 30 YEARS
K/C/O HTN SINCE 20 YEARS
Case History and Clinical Findings
PRESENTING C/O SOB SINCE 4 DAYS
DECREASED URINE OUTPUT SINCE 4 DAYS HOPI:
PATIENT WAS APPARENTLY ASYMPTOMATIC UNTIL 4 DAYS AGO, THEN SHE DEVELOPED SOB , SUDDEN IN ONSET CLASS II PROGRESSED GRADUALLY TO CLASS IV, NOT ASSOCIATED WITH CHEST OPAIN, PALPITATIONS, SWEATING.
NO H/O FEVER, COUGH, RELIEVED WITH NEBULISATION ( DUOLIN)
C/O DECREASED URINE OUTPUT SINCE 4 DAYS, H/O PEDAL EDEMA RELIEVED TO SOME EXTENT WITH ORAL DIURETICS
NO H/O HEADACHE, GIDDINESS, NECK PAIN
NO H/O ORTHOPNEA , PND , SYNCOPE
H/O SIMILAR COMPLAINTS SINCE 4 MONTHS , 3 EPISODES EACH LASTING FOR 15-20DAYS , WHICH SUBSIDES WITH NEBULISATION WITH BRONCHODILATORS AND ORAL DIURETICS PAST HISTORY:
K/C/O TYPE 2 DM SINCE 30 YEARS ON INJ. HAI S/C TID
K/C/O HTN SINCE 2O YEARS ON T. METAPROLOL 50MG/BD + TELMA 40MG /OD K/C/O HYPOTHYROIDIM SINCE 15YEARS ON TAB. THYRONORM 75MCG
K/C/O CKD V
NOT A K/C/O CAD, CVD,TB, ASTHMA ,SEIZURES
PERSONAL HISTORY:- APETITE- NORMAL BOWEL - CONSTIPATION BLADDER - NORMAL ALLERGIES-NIL
ADDICTIONS : CHEWING OF BETEL LEAF SINCE 20 YEARS
FAMILY HISTORY:-NOT SIGNIFICANT GENERAL EXAMINATION:
PT IS CONCIOUS COHERENT AND CO OPERATIVE PALLOR AND PEDAL EDEMA PRESENT
NO ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY JVP RAISED
VITALS:
PR - 86/MIN
BP - 130/70MMHG RR - 22CPM TEMP - 98.7F
SPO2 - 98% AT RA GRBS - 78MG/DL
SYSTEMIC EXAMINATION:
CVS - S1 S2 +, NO MURMURS
RS -BAE+, NVBS , B/L DIFFUSE COARSE CREPTS +
P/A - SOFT , NON TENDER , NO ORGANOMEGALY CNS - GCS - E4V5M6
NO FOCAL NEUROLOGICAL DEFICITS
COURSE IN HOSPITAL:
A 70 YEAR OLD FEMALE CAME WITH ABOVE MENTIONED COMPLAINTS. THOROUGH CLINICAL EVALUATION WAS DONE AND NECESSARY INVESTIGATION WAS SENT. ULTRASOUND WAS DONE AND IMPRESSION SHOWS GRADE 1 RPD CHANGES IN B/L KIDNEYS. PATIENT WAS DIAGNOSED AS ACUTE PULMONARY EDEMA SECONDARY TO LEFT VENTRICULAR FAILURE ( RESOLVED) WITH HEART FAILURE WITH MID RANGE EJECTION FRACTION SECONDARY TO OLD CAD WITH MODERATE IRON DEFICIENCY ANEMIA WITH K/C/O HYPOTHYROIDISM SINCE 15 YEARS WITH K/C/O TYPE 2 DM SINCE 30 YEARS WITH K/C/O HTN SINCE 20 YEARS. OPHTHALMOLOGY REFERAL DONE ON 18/08/24 I/V/O DIABETIC RETINOPATHY CHANGES AND IMPRESSION SHOWS B/E NORMAL FUNDUS STUDY , NO EVIDENCE OF RETINOPATHY CHANGES. ENT REFERAL DONE ON 20/08/24 I/V/O DECREASED HEARING . THEY DIAGNOSED AS B/L IMPACTED WAX AND ADVICED: DEWAX EAR DROPS 4'/4'/4'/4' X 5 DAYS , AVOID MANIPULATION OF EAR ,REVIEW TO ENT OPD AFTER 5 DAYS FOR WAX REMOVAL AND PTA EVALUATION ,CONTINUE MEDICATION AS ADVICED BY PRIMARY PHYSICIAN . DURING THE COURSE PATIENT WAS TREATED WITH ANTIHYPERTENSIVES, DIURETICS, STATINS, THYROID SUPPLEMENTS, ANTIEMETICS, OSMOTIC LAXATIVE AND SUPPLEMENTARY MEDICATION . DURING THE STAY PATIENT IMPROVED CLINICALLY AND IS HENCE BEING DISCHARGED IN HEMODYNAMICALLY STABLE CONDITION.
OPHTHALMOLOGY REFERAL DONE ON 18/08/24 I/V/O DIABETIC RETINOPATHY CHANGES: IMPRESSION:
B/E NORMAL FUNDUS STUDY , NO EVIDENCE OF RETINOPATHY CHANGES.
ENT REFERAL DONE ON 20/08/24 I/V/O DECREASED HEARING DIAGNOSIS : B/L IMPACTED WAX
ADVICED: DEWAX EAR DROPS 4'/4'/4'/4' X 5 DAYS AVOID MANIPULATION OF EAR
REVIEW TO ENT OPD AFTER 5 DAYS FOR WAX REMOVAL AND PTA EVALUATION CONTINUE MEDICATION AS ADVICED BY PRIMARY PHYSICIAN
Investigation
HBsAg-RAPID 17-08-2024 12:30:AM Negative
Anti HCV Antibodies - RAPID 17-08-2024 12:30:AM Non Reactive HEMOGRAM 17/8
HEMOGLOBIN - 7.4 GM/DL
TOTAL COUNT - 10,100 CELLS/CUMM
N/L/E/M/B-75/13/02/10/00 PCV -22.0
MCV-56.3FL MCH-18.9PG MCHC 33.6%
RBC COUNT -3.91MILIONS/CUMM PLATELET COUNT-2.58 LAKHS/CUMM
SMEAR - MICROCYTIC HYPOCHROMIC ANEMIA
RFT 17-08-2024 12:30:AMUREA 90 mg/dl 50-17 mg/dlCREATININE 3.7 mg/dl 1.2-0.6 mg/dlURIC
ACID 3.9 mmol/L 6-2.6 mmol/LCALCIUM 9.9 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 3.5 mg/dl 4.5-2.5
mg/dlSODIUM 133 mmol/L 145-136 mmol/LPOTASSIUM 5.0 mmol/L. 5.1-3.5 mmol/L.CHLORIDE
101 mmol/L 98-107 mmol/L
LIVER FUNCTION TEST (LFT) 17-08-2024 12:30:AMTotal Bilurubin 0.62 mg/dl 1-0 mg/dlDirect Bilurubin 0.18 mg/dl 0.2-0.0 mg/dlSGOT(AST) 48 IU/L 31-0 IU/LSGPT(ALT) 31 IU/L 34-0
IU/LALKALINE PHOSPHATASE 155 IU/L 141-53 IU/LTOTAL PROTEINS 6.5 gm/dl 8.3-6.4
gm/dlALBUMIN 3.96 gm/dl 4.6-3.2 gm/dlA/G RATIO 1.56
ABG 17-08-2024 10:52:AMPH 7.31PCO2 33.9PO2 79.2HCO3 16.8St.HCO3 17.7BEB -8.2BEecf - 8.2TCO2 36.9O2 Sat 94.9O2 Count 8.9
RFT 17-08-2024 10:54:PMUREA 108 mg/dl 50-17 mg/dlCREATININE 4.0 mg/dl 1.2-0.6 mg/dlURIC
ACID 4.84 mmol/L 6-2.6 mmol/LCALCIUM 8.9 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 4.13 mg/dl 4.5-
2.5 mg/dlSODIUM 130 mmol/L 145-136 mmol/LPOTASSIUM 4.4 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 99 mmol/L 98-107 mmol/L
T3, T4, TSH 17-08-2024 10:55:PMT3 0.40 ng/ml 1.87-0.87 ng/mlT4 10.46 micro g/dl 12.23-6.32
micro g/dlTSH 0.78 micro Iu/ml 5.36-0.34 micro Iu/ml TROPONIN I - 8.0PG/ML
RFT 19-08-2024 06:05:AMUREA 113 mg/dl 50-17 mg/dlCREATININE 4.1 mg/dl 1.2-0.6 mg/dlURIC
ACID 5.2 mmol/L 6-2.6 mmol/LCALCIUM 9.1 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 3.7 mg/dl 4.5-2.5
mg/dlSODIUM 132 mmol/L 145-136 mmol/LPOTASSIUM 4.7 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 96
mmol/L 98-107 mmol/L LIPID PROFILE:
TOTAL CHOLESTEROL - 140mg/dl TRIGLYCERIDES - 130mg/dl
HDL CHLESTEROL - 28.8 mg/dl LDL CHOLESTEROL - 84.3 mg/dl VLDL - 26.0
RFT 20-08-2024 06:05:AMUREA 124 mg/dl 50-17 mg/dlCREATININE 4.2 mg/dl 1.2-0.6 mg/dlURIC
ACID 5.3 mmol/L 6-2.6 mmol/LCALCIUM 8.8 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 3.6 mg/dl 4.5-2.5
mg/dlSODIUM 135 mmol/L 145-136 mmol/LPOTASSIUM 4.9 mmol/L. 5.1-3.5 mmol/L.CHLORIDE
101 mmol/L 98-107 mmol/L HEMOGRAM 20/8 HEMOGLOBIN - 6.9GM/DL
TOTAL COUNT - 6,800 CELLS/CUMM
N/L/E/M/B-55/24/04/17/00 PCV -20.9
MCV-57.7FL MCH-19.1PG MCHC 33.0
RBC COUNT -3.62MILIONS/CUMM PLATELET COUNT-2.51 LAKHS/CUMM
SMEAR - MICROCYTIC HYPOCHROMIC ANEMIA WITH MONOCYTOSIS
ULTRASOUND DONE ON 16/08/24:
USG:
PV: NORMAL CBD: NORMAL
GALL BLADDER: DISTENDED PARTIALLY
PANCREAS - NORMAL SIZE AND ECHOTEXTURE , HEAD VISUASLISED. SPLEEN: NORMAL SIZE AND ECHOTEXTURE 8 CM
RT KIDNEY: 8.3 X 4.1 CM LEFT KIDNEY: 8.2X 4.2 CM AORTA IVC: NORMAL
NO ASCITIS
NO LYMPHADENOPATHY
URINARY BLADDER EMPTY ,WALL THICKNESS: NORMAL
V-U JUNCTION - PELVIS COULD NOT BE ASSESED IMPRESSION:
GRADE 1 RPD CHANGES IN B/L KIDNEYS
2D ECHO WAS DONE ON 17/8/24 - IMPRESSION -
RWMA + LAD TERRITORY AND LCD TERRITORY HYPOKINETIC AND RCA HYPOKINESIA MILD TO MODERATE MR+ ( MR JCT AREA 6.0CM2)
MODERATE TR+ WITH MILD PAH ( RVSP = 40+10= 50MMHG) MILD TO MODERATE AR+ (AR-PHT 927 M/SEC )
SCLEROTIC AV , MAC + , NO AS/MS IAS : INTACT : TRIVIAL PR+
EF + 47% MILD LV DYSFUNCTION + GRADE 1 DIASTOLIC DYSFUNCTION +
IVC SIZE ( 1.58CMS) MILD DILATED, INTACT
IVS - 1.25 CM , ESD - 3.48 CM , EDD - 5.20 CM , DPW 1.25 CM
Treatment Given(Enter only Generic Name)
INJ LASIX 40MG IV/BD
INJ. HAI S/C TID A/C TO GRBS
T. TELMA 40 + METAPROLOL 50MG PO/OD
T. METAPROLOL 50MG PO/OD
T. CHLORTHALIDONE 12.5MG PO/OD
T. NITROGLYCERINE 12.5MG PO/BD
T. ATORVASTATIN 40MG PO/HS
T. THYRONORM 75MCG PO/OD SYP. LACTULOSE 30ML PO/BD
SYP. ASCORYL PO/TID 10ML--10ML--10ML
T. SHELCAL CT PO/OD
T. NODOSIS 500MG PO/BD
CAP. BIO D3 PO/OD WEEKLY THRICE
T. OROFER XT PO/OD
Advice at Discharge
INJ. HAI SC TID 6U---6U---6U @ 8AM --- 2PM --- 8PM
T. TELMA 40 + METAPROLOL 50MG PO/OD @ 9AM
T. METAPROLOL 50MG PO/OD @ 9PM
T. NITROGLYCERINE 12.5MG PO/BD @ 9AM---9PM
T. ATORVASTATIN 40MG PO/HS @ 9PM
T. THYRONORM 75MCG PO/OD @ 8AM
T. OROFER XT PO/OD @ 8AM
T. LASIX 20MG PO/BD @ 9M--4PM SYP. LACTULOSE 30ML PO/HS @ 9PM
SYP. ASCORYL PO/TID 10ML--10ML--10ML@ 8AM --- 2PM --- 8PM
Follow Up
REVIEW TO GM OPD AFTER 1 WEEK /SOS
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER
SIGNATURE OF PG/INTERNEE
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
Discharge Date Date: 21/08/24 Ward: FMW Unit:V
Last admission EMR summary
Age/Gender : 78 Years/Female
Address :
Discharge Type: Relieved
Admission Date: 16/11/2024 04:30 AM
Diagnosis
CARDIOGENIC PULMONARY EDEMA ( RESOLVED ) HEART FAILURE WITH PRESERVED EF ( EF - 58 %) RECURRENT UTI
K/C/O HTN K/C/O DM K/C/O CKD
Case History and Clinical Findings C/O PEDAL ODEMA SINCE 2 DAYS C/O SOB SINCE 2 DAYS
PATIENT CAME TO CASUALITY WITH C/0 PEDAL ODEMA 2 DAYS AGO PATIENT WAS APPARENTLY ASSYMPTOMATIC 2DAYS BACK , AFTER WHICH SHE DEVELOPED INSIDIOUS IN ONSET , GRADUALLY PROGRESSIVE PITTING TYPE NO AGGRAVATING AND RELIEVING FACTORS
C/O SOB SINCE 2 DAYS INSIDIOUS IN ONSET GRADUALLY PROGRESSIVE AGGRAVTED ON LYING DOWN, REKLIEVED IN SITING POSITION
C/O DECREASED URINE OUTPUT SINCE YESTERDAY
H/O BURNING MICTURITION SINCE 3 YRS OCCASIONALYY H/O PEDAL ODEMA SINCE 12 YRS
H/O C/O CHEST TIGHTNES
H/O C/O FACIAL PUFFINESS
H/O C/O POLYPHAGIA , POLYDIPSIA , NOCTURIA
PAST HISTORY:
K/C/O DM TYPE 2 SINCE 30 YEARS ON INSULIN K/C/O HTN SINCE 2 YEARS ON MEDICATION
FAMILY HISTORY: NOT SIGNIFICANT
PERSONAL HISTORY:
DIET:MIXED APPETITE:NORMAL SLEEP: ADEQUATE
BOWEL AND BLADDER MOVEMENTS: NORMAL ALLERGIES:NO
ADDICTIONS: NO
GENERAL EXAMINATION:
PT IS C/C/C
NO PALLOR, ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, EDEMA TEMP:AFEBRILE
PR:98 BPM RR:28CPM BP:110/70MMHG SPO2:97% AT RA GRBS:260 MG/DL
SYSTEMIC EXAMINATION: CVS: JVP NOT RAISED CHESTWALL-SYMMETRICAL MOVEMENTS- SYMMETRICAL NO DILATED VEINS
APICAL IMPULSE:- SEEN AT 5TH ICS
S1,S2 HEARD; NO THRILLS , NO MURMURS
RS:BILATERAL AIR ENTRY PRESENT; NORMAL VESCICULAR BREATH SOUNDS HEARD DYSPNOEA +
BILATERAL BASAL CREPTS +
P/A: SOFT, NT, NO ORGANOMEGALY BOWEL SOUNDS HEARD
CNS:NO FOCAL NEUROLOGICAL DEFICIT GCS-E4V5M6
REFLEXES: RIGHT- BICEPS- ++ RICEPS- ++ SUPINATOR- + KNEE- ++ ANKLE- +
LEFT BICEPS- ++ RICEPS- ++
SUPINATOR- + KNEE- ++ ANKLE- +
TONE RIGHT
UL-NORMAL LL-NORMAL LEFT
UL-NORMAL LL-NORMAL
POWER RIGHT UL-5/5 LL-5/5 LEFT UL-5/5 LL-5/5
2D ECHO WAS DONE ON 16/11/2024 FINDINGS:
NO RWMA (? MILD ANTERIOR WALL HYPOKINESIA) MODERATE MR+
MODERATE AR+ SEVERE TR+ WITH PAH
SCLEROTIC AV; MV-THICKENED ; NO AS/MS IAS- INTACT ; CONCENTRIC LVH+
EF=58%, GOOD SYSTOLIC FUNCTION GRADE I DIASTOLIC DYSFUNCTION
IVS SIZE (1.79 CMS) DILATED NON COLLAPSING DILATED RA/ RV/ IVC
MILD DILATED RV
URINE CULTURE AND SENSITIVITYREPORT- E-COLI MORE THAN 10 CFU UNITS /ML IF URINE ISOLATED
AURAL SWAB CULTURE AND SENSITIVITY
REPORT-METHICILLIN RESISTANT STAPHYLOCOCCUS SPP GROWN
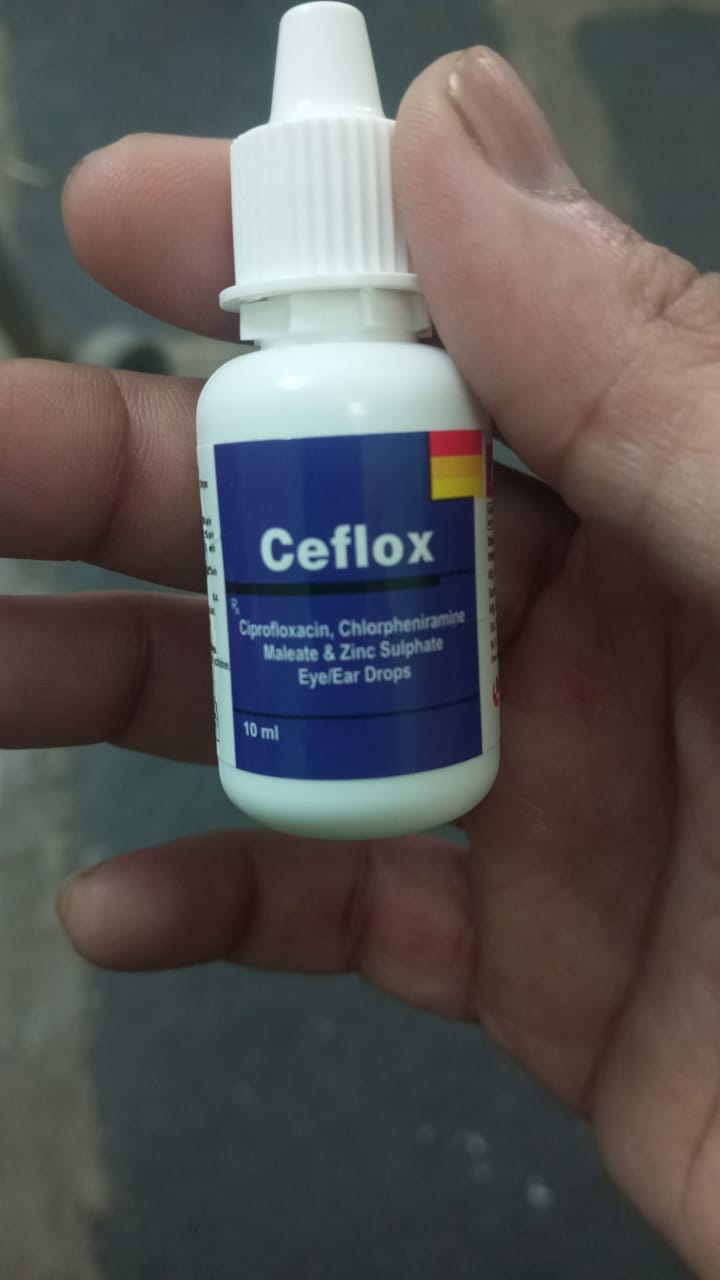
ENT REFERRAL WAS DONE 17/11/2024 I/V/O H/O IMPACTED EAR WAX AND FUNGAL INFECTION
PATIENT WAS ADVICED
1) DEEWAX EAR DROPS QID X 5 DAYS
2) CIPLOX EAR DROPS TID X 5DAYS
Investigation
RFT 16-11-2024 05:49:AMUREA119 mg/dl50-17 mg/dlCREATININE4.0 mg/dl1.2-0.6 mg/dl URIC
ACID4.7 mmol/L6-2.6 mmol/LCALCIUM8.4 mg/dl10.2-8.6 mg/dlPHOSPHOROUS3.5 mg/dl4.5-2.5 mg/dlSODIUM131 mmol/L145-136 mmol/LPOTASSIUM5.3 mmol/L.5.1-3.5 mmol/L.CHLORIDE102 mmol/L98-107 mmol/LLIVER FUNCTION TEST (LFT) 16-11-2024 05:49:AMTotal Bilurubin0.75
mg/dl1-0 mg/dl Direct Bilurubin0.18 mg/dl0.2-0.0 mg/dl SGOT(AST)45 IU/L31-0 IU/LSGPT(ALT)24 IU/L34-0 IU/LALKALINE PHOSPHATASE159 IU/L141-53 IU/LTOTAL PROTEINS5.4 gm/dl8.3-6.4 gm/dlALBUMIN3.27 gm/dl4.6-3.2 gm/dl A/G RATIO1.54COMPLETE URINE EXAMINATION (CUE) 16-11-2024 05:49:AMCOLOURPale yellowAPPEARANCECloudyREACTIONAcidicSP.GRAVITY1.010ALBUMIN++++SUGAR Nil BILE SALTS Nil BILE PIGMENTS Nil PUS CELLS4-6EPITHELIAL CELLS1-2RED BLOOD CELLS1-
2CRYSTALSNilCASTSNilAMORPHOUS DEPOSITS Absent OTHERS Bacteria-present HBsAg- RAPID16-11-2024 10:08:AMNegative Anti HCV Antibodies - RAPID16-11-2024 10:08:AMNon Reactive RFT 17-11-2024 12:02:AMUREA125 mg/dl50-17 mg/dlCREATININE3.9 mg/dl1.2-0.6
mg/dl URIC ACID5.1 mmol/L6-2.6 mmol/LCALCIUM9.2 mg/dl10.2-8.6 mg/dlPHOSPHOROUS3.4 mg/dl4.5-2.5 mg/dlSODIUM132 mmol/L145-136 mmol/LPOTASSIUM5.1 mmol/L.5.1-3.5 mmol/L.CHLORIDE101 mmol/L98-107 mmol/LCOMPLETE URINE EXAMINATION (CUE) 17-11- 2024 07:16:PMCOLOURPale yellowAPPEARANCECloudyREACTIONAcidicSP.GRAVITY1.010ALBUMIN++++SUGAR Nil BILE SALTS Nil Bile PIGMENTS Nil PUS CELLS4-6EPITHELIAL CELLS1-2RED BLOOD CELLS1-
2CRYSTALSNilCASTSNilAMORPHOUS DEPOSITS Absent OTHERS Bacteria-present RFT 18-11- 2024 10:53:PMUREA127 mg/dl50-17 mg/dlCREATININE4.1 mg/dl1.2-0.6 mg/dl URIC ACID5.2
mmol/L6-2.6 mmol/LCALCIUM9.6 mg/dl10.2-8.6 mg/dlPHOSPHOROUS2.9 mg/dl4.5-2.5 mg/dlSODIUM135 mmol/L145-136 mmol/LPOTASSIUM4.7 mmol/L.5.1-3.5 mmol/L.CHLORIDE105 mmol/L98-107 mmol/L
HEMOGRAM: 16/11/2024
HAEMOGLOBIN 6.0 gm/dl 12.0 - 15.0 Colorimetric TOTAL COUNT 8,500 cells/cumm 4000 - 10000
Impedence NEUTROPHILS 88 % 40 - 80 Light Microscopy LYMPHOCYTES 07 % 20 - 40 Light
Microscopy EOSINOPHILS 00 % 01 - 06 Light Microscopy MONOCYTES 05 % 02 - 10 Light
Microscopy BASOPHILS 00 % 0 - 2 Light Microscopy PCV 17.9 vol % 36 - 46 Calculation M C V 57.6 fl
83 - 101 Calculation M C H 19.3 pg 27 - 32 Calculation M C H C 33.5 % 31.5 - 34.5 Calculation RDW-
CV 19.7 % 11.6 - 14.0 Histogram RDW-SD 41.1 fl 39.0-46.0 Histogram RBC COUNT 3.11
millions/cumm 3.8 - 4.8 Impedence PLATELET COUNT 2.08 lakhs/cu.mm 1.5-4.1 Impedence SMEARRBC Microcytic hypochromic Light Microscopy WBC Within normal limits with increased neutrophils Light Microscopy PLATELETS Adequate in number and distribution Light Microscopy HEMOPARASITES No hemoparasites seen Light Microscopy
IMPRESSION Microcytic hypochromic anemia
HEMOGRAM: 17/11/2024
HAEMOGLOBIN 6.2 gm/dl 12.0 - 15.0 Colorimetric TOTAL COUNT 8,000 cells/cumm 4000 - 10000
Impedence NEUTROPHILS 77 % 40 - 80 Light Microscopy LYMPHOCYTES 13 % 20 - 40 Light
Microscopy EOSINOPHILS 01 % 01 - 06 Light Microscopy MONOCYTES 09 % 02 - 10 Light
Microscopy BASOPHILS 00 % 0 - 2 Light Microscopy PCV 17.9 vol % 36 - 46 Calculation M C V 57.0 fl
83 - 101 Calculation M C H 19.7 pg 27 - 32 Calculation M C H C 34.6 % 31.5 - 34.5 Calculation RDW-
CV 19.0 % 11.6 - 14.0 Histogram RDW-SD 39.8 fl 39.0-46.0 Histogram RBC COUNT 3.14
millions/cumm 3.8 - 4.8 Impedence PLATELET COUNT 2.36 lakhs/cu.mm 1.5-4.1 Impedence SMEARRBC microcytic hypochromic Light Microscopy WBC With in normal limits Light Microscopy PLATELETS Adeqaute Light Microscopy HEMOPARASITES No hemoparasites seen Light Microscopy IMPRESSION microcytic hypochromic anemia HEMOGRAM: 18/11/2024
HAEMOGLOBIN 6.1 gm/dl 12.0 - 15.0 Colorimetric TOTAL COUNT 8,800 cells/cumm 4000 - 10000
Impedence NEUTROPHILS 77 % 40 - 80 Light Microscopy LYMPHOCYTES 12 % 20 - 40 Light
Microscopy EOSINOPHILS 01 % 01 - 06 Light Microscopy MONOCYTES 10 % 02 - 10 Light
Microscopy BASOPHILS 00 % 0 - 2 Light Microscopy PCV 17.7 vol % 36 - 46 Calculation M C V 56.5 fl
83 - 101 Calculation M C H 19.5 pg 27 - 32 Calculation M C H C 34.5 % 31.5 - 34.5 Calculation RDW-
CV 20.0 % 11.6 - 14.0 Histogram RDW-SD 40.4 fl 39.0-46.0 Histogram RBC COUNT 3.1
millions/cumm 3.8 - 4.8 Impedence PLATELET COUNT 2.4 lakhs/cu.mm 1.5-4.1 Impedence SMEARRBC Microcytic hypochromic Light Microscopy WBC With in normal limits Light Microscopy PLATELETS Adequate in number and distribution Light Microscopy HEMOPARASITES No hemoparasites seen Light Microscopy IMPRESSION Microcytic hypochromic anemia
Treatment Given(Enter only Generic Name)
IVF NS AT 50 ML/HR
INJ OPTINEURON 1 AMP IN 100ML NS/IV/ OD INJ LASIX INFUSION 3ML / HR IV
INJ HAI SC TID 6U-6U-6U
INJ EPO 4000 IV SC WEEKLY
INJ IRON SUCROSE 20 GMS IN 100 ML NS OVER 40 MIN ALTERNATE DAYS TAB TELMA 40 MG PO/OD
TAB LASIX 20 MG PO / OD
TAB METOPROLOL 50 MG PO /OD TAB OROFER - XT PO / OD
TAB OPTINEURON FORTE PO / OD DEEWAX EAR DROPS
CIPLOX EAR DROPS
Advice at Discharge
INJ HAI SC TID /PREMEAL 6U-6U-6U TO CONTINUE INJ EPO 4000 IV SC WEEKLYTO CONTINUE
TAB LASIX 20 MG PO / BD 8AM-3PMTO CONTINUE TAB OROFER - XT PO / OD 8AMTO CONTINUE
TAB OPTINEURON FORTE PO / OD8AMTO CONTINUE TAB METOPROLOL 25 MG PO /OD8AMTO CONTINUE TAB.AMLODIPINE 5MG PO/OD8AMTO CONTINUE
DEEWAX EAR DROPS 4TIMES 4 DROPS-RIGHT EAR X3 DAYS
Follow Up
REVIEW TO GM AND ENT OP AFTER 5 DAYS /SOS
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER
SIGNATURE OF PG/INTERNEE
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
Discharge Date Date:20 /11/24 Ward:FMW Unit:V
24-11-2024
PPM 1 - There is lot of ear pus discharge today morning....
Here as per sensitivity report ciprofloxacin is resistant and but they given this drops.
As per report cinezolid is showing sensitive....so drops should be taken now.
27-11-2024
PA - Ther is no improvement at all sir evn after giving that antibiotic.
She is having difficulty in swallowing and pain around ear neck and lateral , temporal areas.
What to do sir?
One ENT said as per condition surgery needed.
What scan need to be done sir?
PPM 1 - Review with our ENT for another clinical examination first to decide the next best investigation.
07-12-2024
PA - Good morning sir
Sir there is no relief even after using that linezolid antibiotics...still she complains the same pain n pus n discomfort.
What to do sir ...there is central perforation as per ENT examination.
Sir so what's exact treatment for that ....tympanoplasty?
PPM 1 - What are her
current complaints?
PA - Only Ear pain, Pus discharge, Despite ear drops given.
PPM 1 - What's her daily blood sugar control like?
That needs to br first checked through at least daily fasting and post two hour meal sugars every time she has a meal.
Please let us know those results
PA - Sir ..her health is not good not taking food at all ,want to admit her in your hospital.
PPM 1 - Bring her
PA - Ok sir.
Kindly inform pgs sir.
08-12-2024
PPM 1 - @PPM3 @PPM4 @PPM5 Did this patient get admitted yesterday?
PPM 3 - Patient attender said he would bring her but didn't come sir.
PPM 1 - 👍
18-12-2024
PPM 1 - The patient got admitted again today with increased creatinine this time from 3 to 5 and hyperkalemia of 6.5.
They are unwilling for hemodialysis!
@PPM6 please share the current dextrose insulin doses administered till now and the K+ chart.
21-12-2024
PPM 1 - Update:
Admitted with acute on chronic renal failure with severe metabolic acidosis and encephalopathy necessitating dialysis but discharged as relatives refused dialysis.
Current update:
Sir in private hosp in nalgonda....here after seeing hand color and swelling surgeon saying it may need amputation..and because of multiple puncture improperly blood clot formed clogging the ulnar artery very pain full ...
EMR SUMMARY
Age/Gender : 70 Years/Female
Address :
Discharge Type: Lama
Admission Date: 18/12/2024 10:46 PM
Diagnosis
HEART FAILURE WITH PRESERVED JECTION FRACTION
CKD STAGE 5 WITH HYPERKALEMIA WITH SEVERE METABOLIC ACIDOSIS K/C/O TYPE II DIABETES MELLITUS
K/C/O HYPERTENSION
LEFT CSOM - MUCOSAL TYPE ACTIVE STAGE
Case History and Clinical Findings C/O LEFT EAR PAIN SINCE 15 DAYS C/O PEDAL EDEMA SINCE 10 DAYS HOPI:
PT CAME TO CASUALITY WITH C/O LEFT EAR PAIN SICE 15 DAYS INSISDIOUS IN ONSET GRADUALLY PROGRESSIVE WITH NO AGGRAVATING AND RELEIVING FCATORS
C/O PEDAL EDEMA SINCE 10 DAYS INSISDIOUS IN ONSET GRADUALLY PROGRESSIVE PITTING TYPE WITH NO AGGRVATING AND RELEIVING FACTORS
H/O BURNING MICTURITION SINCE 3 YEARS OCCASIONALLY H/O PEDAL EDEMA SINCE 12 YEARS
H/O FACIAL PUFFINESS SINCE 12 YEARS OCASSIONALLY H/O POLYPHAGIA, POLYDIPSIA, NOCTURIA
H/O IMPACTED EAR WAX AND FUNGAL INFECTION FOR WHICH AURAL SWAB WAS SENT WHICH SHOWED METHICILLIN RESISTANT STAPHYLOCOCCI
PAST HISTORY:
K/C/O DM 2 SINCE 30 YEARS AND ON INSULIN K/C/O HTN SONCE 2 YEARS AND ON MEDICATION NO OTHER COMORBIDITIES
APETITE LOST SINCE 1 MONTH BURNING MICTURITION
ON EXAMINATION :
PT IS C/C/C
NO PALLOR,ICTERUS,CYNOSIS, LYMPHADENOPATHY,ODEMA,CLUBBING. HT- 154CM, WT- 52KGS, BMI- 23.6KG/M2
TEMPERATURE - AFEBRILE PR 80BPM
RR 16CPM BP: 100/60MMHG SPO2: 99@ RA
GRBS 85MG/DL SYSTEMIC EXAMINATION
CVS : S1S2 HEARED , NO MURMURS
RS : NVBS, BILTERAL AIRWAY ENTRY PRSENT ABDOMEN : SOFT AND NON TENDER CNS:NFND, GLASSGOW COMA SCALE E4V5M6
NEPHROLOGY REFERRAL WAS DONE ON 19/12/24 I/V/O DERANGED RFT AND ABG ADVISE-
FLUID RESTRICTION <1.5LT/DAY SALT RESTRICTION <2G/DAY
NEB WITH LEVOSALBUTAMOL 4 RESP STAT
INJ. CALCIUM GLUCONATE 1 AMP IV 100ML NS IV OVER 10 MINS INJ. HAI IN 25D IV OVER 1 HR
TAB. LASIX 40MG IV/BD
INJ SODIUM BICARBONATE 100MEQ IN 200ML NS IV OVER 6 HRS TAB. NODOSIS 1 GM PO/TID
TAB. SHELCAL- CT PO/OD TAB. OROFER-XT PO/OD
INJ. EPO 4000IU/SC ONCE A WEEK CAP BIO-D3 PO/OD ONCE A WEEK STRICT I/O MONITORING
MONITORS VITALS AND INFORM SOS
ENT REFERRAL WAS DONE ON 20/12/24 I/V/O H/O LEFT EAR WAX (IMPACTED) AND FUNGAL INFECTION OF LEFT EAR
ADVISE- LEFT AURAL SWAB FOR C/S TREATMENT- TAB CIPLOX EAR DROPS X 5 DAYS TAB LEVOCET 5MG OD/HS X 5 DAUS
DEWAX EAR DROPS X 5 DAYS REVIEW WITH CLTURE REPORTS
Investigation
RFT 18-12-2024 11:30:PMUREA 160 mg/dl 50-17 mg/dlCREATININE 5.4 mg/dl 1.2-0.6 mg/dlURIC
ACID 9.8 mmol/L 6-2.6 mmol/LCALCIUM 8.5 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 5.6 mg/dl 4.5-2.5
mg/dlSODIUM 132 mmol/L 145-136 mmol/LPOTASSIUM 6.5 mmol/L. 5.1-3.5 mmol/L.CHLORIDE 99
mmol/L 98-107 mmol/L
LIVER FUNCTION TEST (LFT) 18-12-2024 11:30:PMTotal Bilurubin 1.70 mg/dl 1-0 mg/dlDirect Bilurubin 0.65 mg/dl 0.2-0.0 mg/dlSGOT(AST) 632 IU/L 31-0 IU/LSGPT(ALT) 292 IU/L 34-0
IU/LALKALINE PHOSPHATASE 196 IU/L 141-53 IU/LTOTAL PROTEINS 5.2 gm/dl 8.3-6.4
gm/dlALBUMIN 3.29 gm/dl 4.6-3.2 gm/dlA/G RATIO 1.72HBsAg-RAPID 18-12-2024 11:30:PM
Negative
Anti HCV Antibodies - RAPID 18-12-2024 11:30:PM Non ReactiveABG 19-12-2024 08:18:AMPH 7.10PCO2 20.7PO2 91.3HCO3 6.3St.HCO3 8.2BEB -21.6BEecf -21.5TCO2 14.6O2 Sat 93.2O2
Count 8.2
SERUM ELECTROLYTES (Na, K, C l) 19-12-2024 12:09:PMSODIUM 126 mmol/L 145-136
mmol/LPOTASSIUM 6.7 mmol/L 5.1-3.5 mmol/LCHLORIDE 95 mmol/L 98-107 mmol/L
RFT 19-12-2024 11:40:PMUREA 183 mg/dl 50-17 mg/dlCREATININE 6.3 mg/dl 1.2-0.6 mg/dlURIC
ACID 10.0 mmol/L 6-2.6 mmol/LCALCIUM 9.0 mg/dl 10.2-8.6 mg/dlPHOSPHOROUS 6.3 mg/dl 4.5-
2.5 mg/dlSODIUM 128 mmol/L 145-136 mmol/LPOTASSIUM 5.8 mmol/L. 5.1-3.5 mmol/L.CHLORIDE
100 mmol/L 98-107 mmol/L
LIVER FUNCTION TEST (LFT) 19-12-2024 11:40:PMTotal Bilurubin 2.04 mg/dl 1-0 mg/dlDirect Bilurubin 0.98 mg/dl 0.2-0.0 mg/dlSGOT(AST) 1331 IU/L 31-0 IU/LSGPT(ALT) 725 IU/L 34-0
IU/LALKALINE PHOSPHATASE 205 IU/L 141-53 IU/LTOTAL PROTEINS 5.2 gm/dl 8.3-6.4 gm/dlALBUMIN 3.29 gm/dl 4.6-3.2 gm/dlA/G RATIO 1.72ABG 20-12-2024 07:15:AMPH 7.238PCO2
19.3PO2 211HCO3 7.9St.HCO3 10.4BEB -18.2BEecf -18.2TCO2 18.0O2 Sat 98.6O2 Count 8.3 HEMOGRAM: 19/12/24
HB- 7.3
TLC- 14000
RBC- 3.75
PLT COUNT- 80000
HEMOGRAM: 20/12/24 HB- 6.3
TLC- 18800
RBC- 3.05
PLT COUNT- 62000
Treatment Given(Enter only Generic Name)
INJ. NORAD 8MG IN 50ML @ 3.5ML/HR TO MAINTAIN MAP >/= 65MMHG INJ 25DEXTROSE WITH 8 UNITS HAI IV/TID OVER 15-20 MINS
INJ CALCIUM GLUCONATE 1 AMP IN 100ML NS IV/TID OVER 15 MINS INJ HAI SC/TID ACC TO GRBS
INJ LASIX 40MG IV/BD IF SYS BP IS >/= 110MMHG TAB ISOLAZINE 1/2 TAB PO/TID
TAB METAPROLOL 25MG PO/OD TAB AMLODIPINE 5MG PO/OD TAB OROFER-XT PO/OD
TAB OPTINEURON 40 PO/OD
K BIND SACHET IN 1 GLASS OF WATER PO/TID NEB WITH 4 RESPULES SALBUTAMOL QID TAB NODOSIS 500MG PO/TID
Advice at Discharge
LAMA NOTES -
PATIENT ATTENDERS HAVE BEEN EXPLAINED ABOUT THE CONDITION OF THE PATIENT THAT IS HEART FAILURE WITH PRESERVED EJECTION FRACTION ,CHRONIC KIDNEY DISEASE STAGE 5 WITH HYPERKALEMIA ,SEVERE METABOLIC ACIDOSIS K/C/O TYPE 2 DM,HTN,LEFT CSOM.THE RISKS AND COMPLICATIONS ASSOCIATED WITH HER CONDITION LIKE ARRHYTHMIAS ,ACUTE PULMONARY EDEMA,SUDDEN CARDIAC ARREST HAVE BEEN EXPLAINED.THE NEED FOR HEMODIALYSIS HAS BEEN EXPLAINED ALONG WITH THE RISKS AND COMPLICATIONS DURING THE PROCEDURE BUT PATIENT ATTENDERS ARE NOT WILLING FOR HEMODIALYSIS AND FURTHER MANAGEMENT AND WANTS TO LEAVE AGAINST MEDICAL ADVISE .HOSPITAL STAFF,DOCTORS, NURSES ARE NOT RESPONSIBLE FOR ANY UNTOWARD EVENTS AFTER LEAVING THE HOSPITAL
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE,DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration : - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER
SIGNATURE OF PG/INTERNEE
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
Discharge Date Date:20/12/24 Ward: ICU
Unit:III



















No comments:
Post a Comment