THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HER SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY EXPERTS WITH AN AIM TO SOLVE THOSE PATIENT'S CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUTS.
56F Abdominal pain 5 years, ileal perforation 1year, Lump abdomen 1 month.
December 28, 2023
*56yr/F housewife married at the age 24yrs after 1yr she gave birth to 1daughter (1994 - lscs) yrs she gave birth to another daughter (lscs-1996)
*After 5yrs in 2001 Tubectomy was done.
18yrsbacks (*In 2005) she was diagnosed with hypothyroidism and was on medication thyronorm since then started on 50mcg initially, later on 75mcg now currently on 62.5 mcg/OD.
In *July 2020 she had 2 episodes of dark colored stools and pain abdomen and incomplete evacuation.
-USG ABDOMINEN showed - multiple enlarged Retroperitoneal and mesenteric lymph nodes (? infective/inflammatory/? T. B
-Colonoscopic Biopsy taken from terminal ileum ulcer and HPE showed dense inflammatory cell infiltrate comprising predominantly lymphocytes with neutrophils, with no necrosis and granulomas to confirm T. B.)
-mantoux test - 28mm & biopsy for gene expert negative.
*20/8/2020 ATT was started.
*In August 2021 ie after 1yr ATT was stopped (colonoscopy was repeated After stopping ATT which showed normal study with no ulcers) pt improved symptomatically.
After 18 months ie in MAY 2023 pt had pain abdomen and Xray showed air under diaphragm, emergency exploratory laparotomy was done i/v/o terminal ileum perforation.
Now From NOV 2023 ie 5months after the surgery pt is again having intermittent pain abdomen, with swelling in left iliac region
(CECT abd showing an ill defined soft tissue
Density adherent to ant. abdominal wall s/o
? Focal omental necrosis/infarct? Focal
Omental infective lesion and umbilical hernia with omentum as content).
Original case report link👇
History of presenting illness-patient was apparently asymptomatic 6 months ago then she was diagnosed to had intestinal obstruction for which she got operated. Now she has complaints of left iliac fossa pain since 3 months aggregated since 10 days pricking type of pain continuous and associated with fever.
No h/o vomiting, diarrhoea
No h/o blood in urine, Malena, no h/o headache, dizziness.
No h/o SOB, palpitations, chest pain.
K/c/o intestinal TB 3 years ago (used ATT medication for 1year)
K/c/o hypothyroidism 10 years ago on thyronorm 50 MCG
K/c/o CAD 6 months aho
N/k/c/o hypertension, diabetes, asthma, epilepsy.
Treatment history
Sx laparotomy for iliac perforation.
Personal history:
Diet: Mixed
Appetite: normal
Sleep: adequate
Bowel and bladder movements: regular
No significant family history
General Examination:
Patient is conscious, coherent and cooperative
Moderately built and nourished
Pallor, icterus, cyanosis, clubbing, Lymphadenopathy -absent
Bilateral pedal edema subsided
Vitals:
PR: 86 bpm
BP: 110/80 mmHg
RR: 16CPM
Temperature: 98.6F
Spo2: 98 % on RA
GRBS-162 mg/dl
Weight:55kg
SYSTEMATIC EXAMINATION
Abdominal examination
P/A-
Shape of abdomen-obese
Tenderness- present in left iliac fossa
Palpable mass -No
Hernial orifices-normal
Free fluid - No
Bruits- No
Liver - Not palpable
Spleen- Not palpable
Bowel sounds- heard
Cardiovascular system examination
Jvp not raised
Inspection:
Shape of chest - elliptical
No visible pulsations
No engorged veins and scars
Apical impulse not visible
Thrills-no
Cardiac sounds- S1S2 heard
No murmurs
Respiratory System -
Dyspnoea- no
Wheeze- No
Trachea position- central
No adventitious sounds.
CVS
Level of consciousness-conscious
Speech- normal
No signs of meningeal irritation.
Motor system:
Rt- UL. LL. Lt- UL. LL
Bulk - normal N. N. N
Tone - N. N. N. N
Power - 5/5. 5/5. 5/5. 5/5
Reflexes:
UL LL
Biceps . 2+. 2+
Triceps. 2+. . 2+
Supinator. 2+. 2+
Knee 2+. 2+
Ankle. 2+. 2+
Sensory system: intact
Coordination is present
Gait is normal
No Cerebellar signs
Investigations
24/12/2023

25/122023
After potassium correction
APRIL 2023 CECT SCAN
DECEMBER 2023 CECT SCAN
Rectus sheath abscess aspiration
Differential diagnosis
Intestinal tuberculosis
Chrons disease
Provisional diagnosis
Chrons disease
[7.10 am, 06/01/2026] PPM 1: Update from the patient advocate:



[7.13 am, 06/01/2026] PPM 1: I tried checking the case report in the link but it doesn't mention much except that we had thought about Crohn's at that time when she was admitted. Hope I recall there was much more to the case than in the case report and I'll need to see if I can fish out her EMR summary from the hospital computer today.
[10.40 am, 07/01/2026] PPM 1: EMR summary
Age/Gender: 58 Years/Female
Address:
Discharge Type: Relieved
Admission Date: 24/12/2023 01:59 PM
Discharge Date: 08/01/2024 04:02 PM
Diagnosis
RECURRENT INTESTINAL OBSTRUCTION DUE TO INTESTINAL INFLAMMATORY DISEASE 3 YEARS BACK, TREATED AS Empirical TUBERCULOSIS, ILEAL PERFORATION FOLLOWING 1 BOUT OF INTESTINAL OBSTRUCTION 3 MONTHS BACK ILEAL PERFORATION SEALED WITH OMENTAL PATCH, WHICH LATER DEVELOPED INTO
OMENTAL ABSCESS GRANULOMA DUE TO SILK SUTURES OMENTAL STITCH ABSCESS AND GRANULOMA REMOVED SURGICALLY AFTER LAPAROSCOPY ISSUES PENDING - RECURRENT INTESTINAL Obstruction DUE TO? ILEAL STRICTURES, THAT NEED TO BE IMAGED BY ENTEROCLYSIS, AND FURTHER DESCISION FOR
ILEOPLASTY OR CONSERVATIVE MANAGEMENT
Case History and Clinical Findings
A 56 YEAR OLD FEMALE HAVE COMPLAINTS OF PAIN ABDOMEN SINCE 10 DAYS
HISTORY OF PRESENTING ILLNESS-PATIENT WAS APPARENTLY ASYMPTOMATIC 6
MONTHS AGO, THEN SHE WAS DIAGNOSED TO HAD INTESTINAL OBSTRUCTION FOR WHICH SHE GOT OPERATED.NOW SHE HAS COMPLAINTS OF LEFT ILIAC FOSSA PAIN SINCE 3 MONTHS AGGRAVATED SINCE 10 DAYS PRICKING TYPE OF PAIN CONTINUOUS AND ASSOCIATED WITH FEVER.
NO HO VOMITING, DIARRHEA
Page-2
KIMS HOSPITALS
NO H/O BLOOD IN URINE, MALENA, NO H/O HEADACGE, DIZZINESS.
NO H/O SOB, PALPITATIONS, CHEST PAIN.
K/C/O INTESTINAL TB 3 YEARS AGO (USED ATTMEDICATION FOR 1YEAR)
K/C/O HYPOTHYROIDISM 10 YEARS AGO ON THYRONORM 50 MCG
K/C/O CAD 6 MONTHS AHO
N/K/C/O HYPERTENSION, DIABETES, ASTHMA, EPILEPSY.
TREATMENT HISTORY
SX LAPAROTOMY FOR ILIAC PERFORATION.
PERSONAL HISTORY:
DIET :MIXED
APPETITE : NORMAL
SLEEP: ADEQUATE
BOWEL AND BLADDER MOVEMENTS: REGULAR
NO SIGNIFICANT FAMILY HISTORY
GENERAL EXAMINATION:
PATIENT IS CONSCIOUS, COHERENT AND COOPERATIVE
MODERATELY BUILT AND NOURISHED
PALLOR, ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY -ABSENT
BILATERAL PEDAL EDEMA SUBSIDED
VITALS:
PR: 86 BPM
BP: 110/80 MMHG
RR: 16CPM
TEMPERATURE: 98.6F
SPO2: 98 % ON RA
GRBS-162 MG/DL
WEIGHT:55KG
SYSTEMATIC EXAMINATION
ABDOMINAL EXAMINATION
P/ASHAPE.
OF ABDOMEN-OBESE
Page-3
KIMS HOSPITALS
TENDERNESS- PRESENT IN LEFT ILIAC FOSSA
PALPABLE MASS -NO
HERNIAL.ORIFICES-NORMAL
FREE FLUID - NO
BRUITS- NO
LIVER - NOT PALPABLE
SPLEEN- NOT PALPABLE
BOWEL.SOUNDS- HEARD
CARDIO VASCULAR SYSTEM EXAMINATION
JVP NOT RAISED
INSPECTION:
SHAPE OF CHEST - ELLIPTICAL
NO VISIBLE PULSATIONS
NO ENGORGED VEINS AND SCARS
APICAL IMPULSE NOT VISIBLE
THRILLS-NO
CARDIAC SOUNDS- S1S2 HEARD
NO MURMURS
RESPIRATORY SYTEM -
DYSPNOEA- NO
WHEEZE- NO
TRACHEA POSITION- CENTRAL
NO ADVENTITIOUS SOUNDS.
CVS
LEVEL OF CONSCIOUSNESS-CONSIOUS
SPEECH- NORMAL
NO SIGNS OF MENINGEAL IRRITATION.
MOTOR SYSTEM: RT-UL. LL. LT- UL. LL
BULK - NORMAL N. N. N
TONE - N. N. N. N
POWER - 5/5. 5/5. 5/5. 5/5
REFLEXES: UL LL
BICEPS. 2+. 2+
Page-4
KIMS HOSPITALS
TRICEPS. 2+. . 2+
SUPINATOR. 2+. 2+
KNEE 2+. 2+
ANKLE. 2+. 2+
SENSORY SYSTEM: INTACTCO ORDINATION IS PRESENTGAIT IS NORMALNO CEREBELLAR
SIGNS
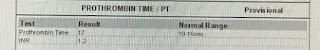
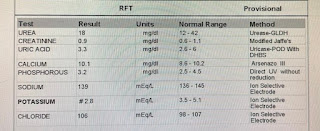
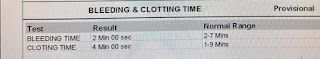
Investigation
RFT UREA 18 mg/dl
CREATININE 0.9 mg/dl
URIC ACID 3.3 mg/dl
CALCIUM 10.1 mg/dl
PHOSPHOROUS 3.2 mg/dl
SODIUM 139 mEq/L
POTASSIUM 2.8 mEq/L
CHLORIDE 106 mEq/L
LIVER FUNCTION TEST (LFT)
Total Bilurubin 0.68 mg/dl
Direct Bilurubin 0.18 mg/dl
SGOT(AST) 17 IU/L
SGPT(ALT) 23 IU/L
ALKALINE PHOSPHATE 183 IU/L
TOTAL PROTEINS 7.6 gm/dl
ALBUMIN 3.82 gm/dl
A/G RATIO 1.01
COMPLETE BLOOD PICTURE (CBP)
HAEMOGLOBIN 10.2 gm/dl
TOTAL COUNT 9100 cells/cumm
NEUTROPHILS 70 %
LYMPHOCYTES 24 %
EOSINOPHILS 02 %
MONOCYTES 04 %
BASOPHILS 00 %
Page-5
KIMS HOSPITALS
PLATELET COUNT 3.7
SMEAR Normocytic normochromic anemia
COMPLETE URINE EXAMINATION (CUE)
COLOUR Pale yellow
APPEARANCE Clear
REACTION Acidic
SP.GRAVITY 1.010
ALBUMIN Nil
SUGAR Nil
BILE SALTS Nil
BILE PIGMENTS Nil
PUS CELLS 2-4
EPITHELIAL CELLS 2-3
RED BLOOD CELLS Nil
CRYSTALS Nil
CASTS Nil
AMORPHOUS DEPOSITS Absent
OTHERS Nil
HBsAg-RAPID Negative
Anti HCV Antibodies - RAPID Non Reactive
SERUM ELECTROLYTES (Na, K, C l) AND SERUM IONIZED CALCIUM
SODIUM 144 mEq/L
POTASSIUM 4.0 mEq/L
CHLORIDE 104 mEq/L
CALCIUM IONIZED 1.31 mmol/L
T3, T4, TSH
T3 1.47 ng/ml
T4 17.96 micro g/dl
TSH 8.915 micro Iu/ml
SERUM ELECTROLYTES (Na, K, C l) AND SERUM IONIZED CALCIUM
SODIUM 146 mEq/L
POTASSIUM 2.7 mEq/L
Page-6
KIMS HOSPITALS
CHLORIDE 102 mEq/L
CALCIUM IONIZED 1.03 mmol/L
SERUM ELECTROLYTES (Na, K, C l) AND SERUM IONIZED CALCIUM
SODIUM 143 mEq/L
POTASSIUM 3.8 mEq/L
CHLORIDE 102 mEq/L
CALCIUM IONIZED 1.24 mmol/L
CYTOLOGY - BODY FLUID (RECTUS SHEATH ABSCESS)
IMPRESSION - FEATURES SUGGESTIVE OF ACUTE INFLAMMATORY LESION - ABSCESS
Treatment Given(Enter only Generic Name)
TNJ MAGNEX FORTE 1.2 GM IV BD
T PAN 40 MP PO OD
T HIFENAC P PO BD
T CHYMORAL FORTE PO TID
T MVT PO OD
T VIT C PO OD
T NITROLONG 2.6 MG PO BD
T THYRONORM 50 MCG PO OD
T ATORVASTATIN 10 MG PO OD
SYP CREMAFFFIN 20 ML PO HS
OINT SMUTH FO L/A
SITZ BATH WITH BETADINE FOR 10 MIN QID
Advice at Discharge
T VIT C PO OD X 15 DAYS
T MVT PO OD X 15 DAYS
T THYRONORM 50 MCG PO OD
T NITROLONG 2.6 MG PO BD
T ATORVA 10 MG PO OD
T CLOPIDOGREL 75 MG PO OD
SYP CREMAFFIN 20 ML PO BD
OINT SMUTH FOR L/A
Page-7
KIMS HOSPITALS
SITZ BATH WITH BETADINE FOR 10 MIN QID
AVOID LIFTING HEAVY WEIGHTS
ABDOMINAL BINDER
HIGH FIBRE DIET
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE, DONOT MISS MEDICATIONS. In case of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendant Declaration: - The medicines prescribed
and the advice regarding preventive aspects of care, when and how to obtain urgent care have been
explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER
SIGNATURE OF PG/INTERNEE
SIGNATURE OF ADMINISTRATOR
SIGNATURE OF FACULTY
Discharge Date
Date:9/1/24
Ward: SSW
Unit:5
[8.28 am, 21/01/2026] PPM 1: Today's update with CT abdomen report [20/01, 17:56]hu1: Sir patient er CT abdomen er report
[20/01, 22:39]hu1: Sir kchu khrap ache ki??
[21/01, 07:32]hu2: Na
[21/01, 07:39]hu1: Sir eta thle akhon ki kra jabe??
[21/01, 07:40]hu1: Diet chart follow kore r excercise kore ki treat kora jabe?
[21/01, 07:57]hu2: Diet and exercise is for her abdominal fat which is pushing the hernia through the hole in the abdominal wall visible on CT (please share the images).
To close the hole one would need to suture the hole aka hernia surgery
[21/01, 08:00]hu1: Okk sir
[21/01, 08:20]hu2: Please share the CT abdomen images















No comments:
Post a Comment