19-09-2024
This is an online E Log book to discuss our patient's de-identified health data shared after taking her signed informed consent. Here we discuss our patients problems through series of inputs from available global online community experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
To begin with, the patient was hale and healthy at the time of her marriage weighing more than 85kg. Later she had two children, one boy and girl. She had gone for abortion twice. She was hard working lady and was a commerce lecturer. She was a tutor to B.Com students. Since 2013 she was suffering with diarrhoea for which she quit her job.
In 2015 she got hernia surgery done and the same day her son left to US for further career growth.
Later she experienced severe body pains and was diagnosed with Rheumatoid arthritis. She was prescribed Methotrexate 7.5mg per week. Alongwith anemia was also treated. Slowly she became weak and there was no respite from diarrhoea. She was advised to stop Methotrexate for which she had some relief from weakness.
But there was no stopping of diarrhoea problem. She suffered with diarrhoea for 11yrs continuously.
Later a gastroenterology surgeon performed colonoscopy and Biopsy, by which she was diagnosed with intestinal TB and was treated with the below medicines.
Tab.Ethambutal
Tab.Refampin
Tab.Isoniagid
Tab.Pyraginamide 900mg.
She Later developed liver problems and her SGOT and SGPT increased. Then she was advised to stop prescribed medicines and was given Streptomycin injection. Later her Serum Creatinine increased and one of her Kidney was damaged. She was in ICU for two days and later discharged.
She was advised to stop Streptomycin. Once again she consulted gastroentrologist and was prescribed TB medication. Fed up with all this prolonged illness she stopped all medications except Pantaprazole. In all these years with all these medications and treatment she lost apetite since 2yrs and was drastically reduced to 34.5kg. She was admitted in ICU on October 18th, 2024. At the time of admission she was almost in coma. She survived in ICU for 5days. She was given CPR on her first cardiac arrest and could not survive on second cardiac arrest.
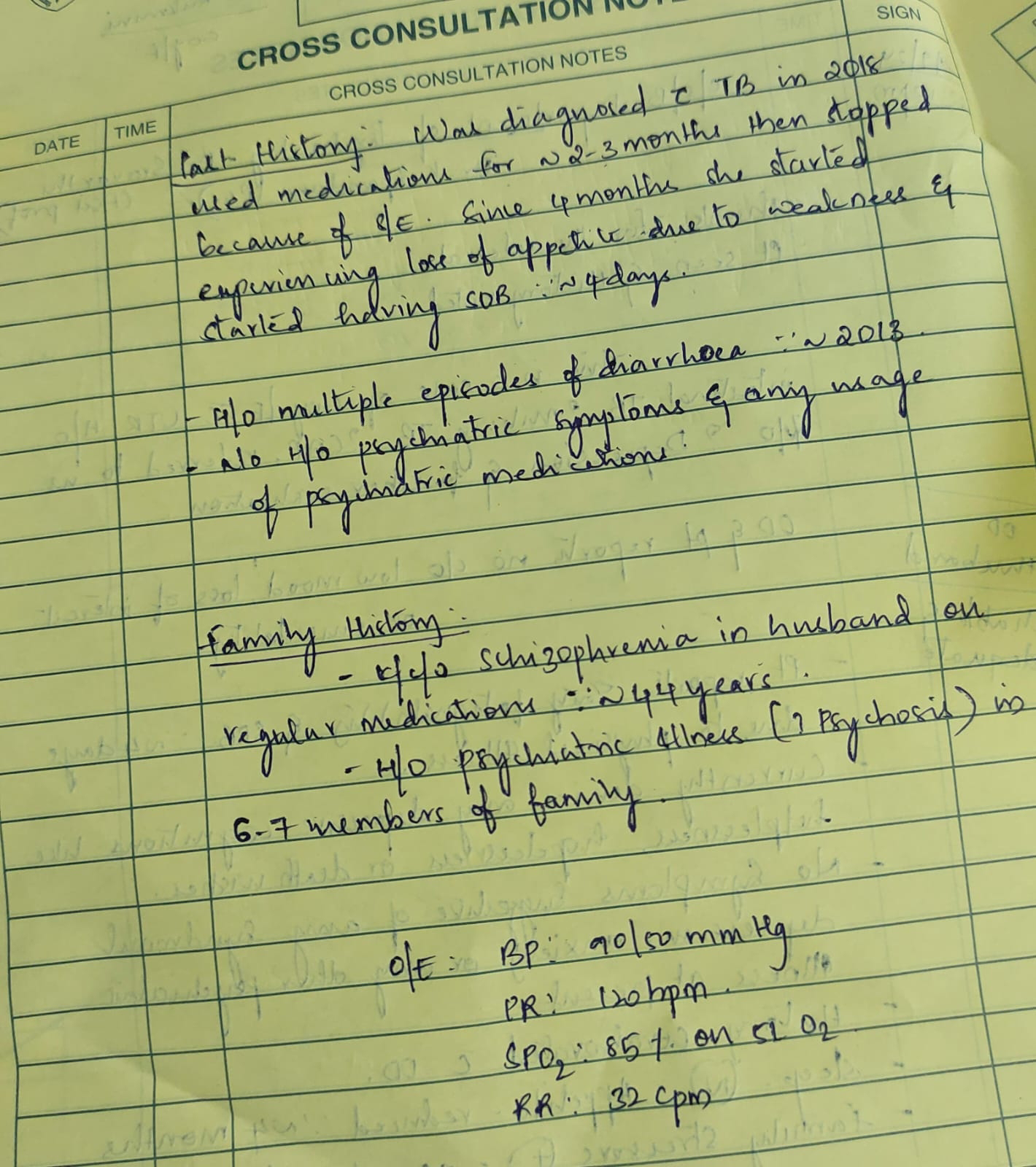
PATIENT HISTORY AT THE TIME OF ADMISSION
The patient was first treated with Methotrexate 5yrs back due to body pains.
Later she got severe diarrhoea. She got done colonoscopy and biopsy- Diagnosed as intestinal TB. Given 900mg tablet with 4 drugs(ethabutal, isoniagid, recompile and one more drug. Due to side effects SGOT and SGPT increased so stopped the tablets and given Streptomycin and one more antibiotic for one month. After one month she got balance problem. She stopped these antibiotics also. Out of fear she stopped taking medicines since 2yrs.
Since 4 days she got cough and is not able to eat food since 2 days.
18-09-2024
PPM 1 - Can I prepare her group and take appointment from PPM2. Can I inform administration about this visit as it will be done during our official duty hours?
PA - OK Sir please prepare. She is afraid of giving blood every time for tests, please minimise the procedure. She is asking for bath.
PPM 1 - Good sign.
PA - 3yrs back they did endoscopy and said inflammation is there in esophagus. Pantaprazole not required sir? From 2yrs she is taking continuously
PPM 1 - Not required. Yes vitamins will be surely given.
PA - Prior to Methotrexate also she is having diarrhoea sir. Kept riles tube. If she is taking any food she is passing gas with foul smell.
PPM 1 - No problem. That means the intestine has started moving.
PA - OK Sir.
PPM 1 - She appears to be having hyperglycemia documented here for the first time and she hasn't received anything other than NS! Now on further history taking she is a known diabetic since 15yrs.
@PPM2 Pease start 6U of soluble Insulin thrice daily before the RT feeds and 4U of NPH twice daily and get regular seven point sugar profile to titrate the dose.
PPM 2 - OK Sir
PPM 1 - @PPM3 Please share what is good time for the patient to call you for the PNI evaluation.
PPM 3 - Sir today at 7 pm.
PA - OK Sir, is iron required for blood transfusion?
PPM 1 - Yes oral iron was advised @PPM2. Injection vitamin B12 will be more helpful as well.
PA - BP has slightly increased sir. Now it is 100/50.
PPM 1 - @PPM2 Look for iron syrup or liquid preparation and adjust the dose as per body weight. Please share her body weight.
Participant 20 - Hopeful screening for Z is being considered? Still remember it is usually done for allTB patients I think.
PA - Still cough is there. There is more sputum and have collected. She is having loose stools if eating anything. Her esophagus has inflammation. Today milk Ragi malt and fluconazole tablet also given through riles tube sir. That's why she is passing loose stools 3-4 times. Her sugar levels are high sir. Should not give milk with sugar?
PPM 1 - Yes don't add sugar in anything.
@PPM2 plan for the upper GI endoscopy tomorrow.
PPM 2 - OK Sir.
PA - We are giving through riles tube. She passed stools 5 times. She is passing stools more times if eating anything.
PPM 1 - Good news.
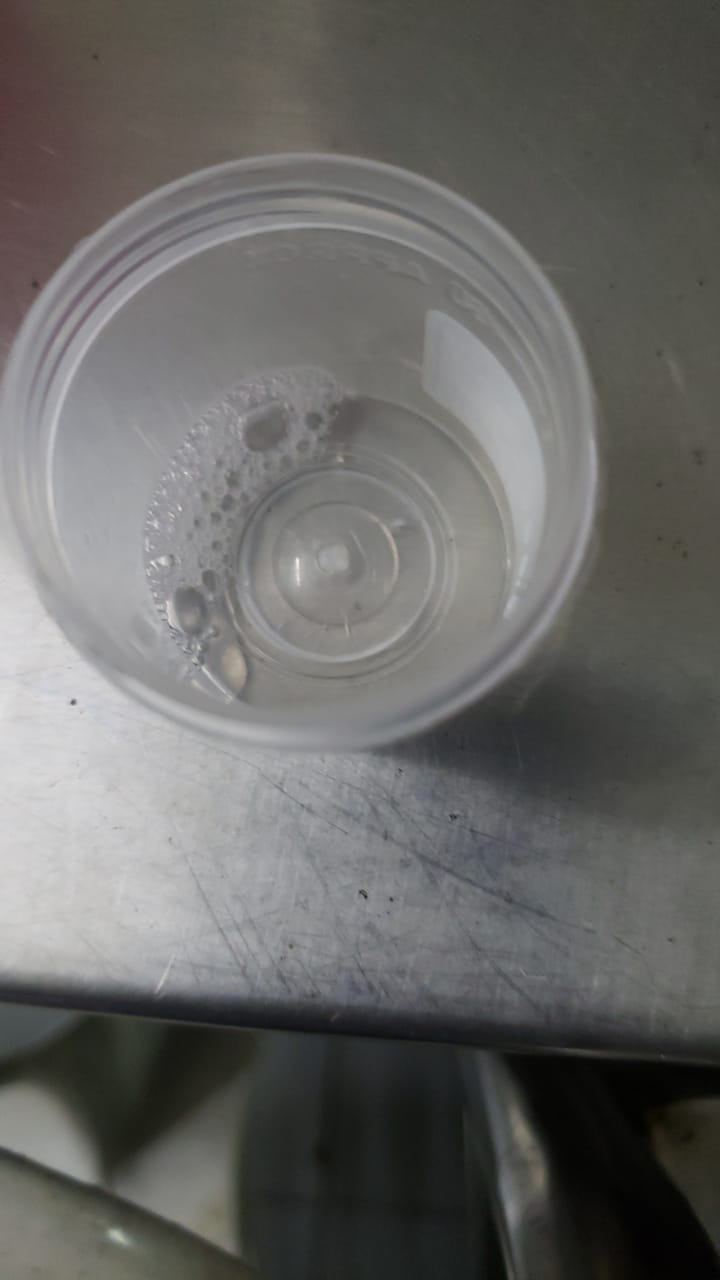
One thing we ask all our patients with lung symptoms to do is to collect their 24hrs sputum everyday from 9.am in a glass and share the image at the end of 9.am next day as it helps us to macroscopically monitor the bronchial inflammation if any.
Here's a case report where it has been well archived.
https://ssaha15.blogspot.com/2023/02
medical-case.html.
PA - Collected the sputum sir.
PPM 4 - Send pic of it.
PA - OK Sir. Will send later.
PPM 1 - Can share a pic anytime but keep collecting it in a glass till 9.am tomorrow and share the image of the 24hr sputum.
PA - OK Sir
PPM 2 - Sir her hb is 3.4gm/dl
PPM 1 - That's not really a contra indication unless we suspect an ongoing fresh upper GI bleed that can be reflected in the postural drop of blood pressure. Also a clear riles tube aspirate rules out a major upper GI bleed. But it's okay even if it's not done as it's largely to look at her esophageal candidates.
PPM 2 - It's clear sir
PA - Blood volume and hemoglobin percentage, both are different sir?
PPM 1 - Yes she likely has Chronic anemia.
PA - Yes sir probably. She is having Thums UP daily for glucose. I couldn't stop her.
PPM - 4 Sir could the diarrhoea she experienced be worsened because of Methotrexate she was on? Were there any other symptoms s/o intestinal TB that time? What were her TLCs and HB after Methotrexate sir? And what was the nature of stools that time? Was it s/o small volume or large volume., a/w any blood or mucus?? Did we see the previous colonoscopy and biopsy report? Was it a definite proven intestinal TB? The loose stools she has since 2 days as I can see from the pulmoreferral notes is same as the loose stools she experienced before??
Does she have any dysphagia or odynophagia s/o esophageal candidates sir?? The inflammation in the endoscopy could be a reflux symptom for which she was given Pantaprazole??
PA - Sir from 2013 she had diarrhoea. Because of this problem she quit the job. In 2015 she had hernia surgery. Later she had severe body pains for which an anaesthesias gave her Methotrexate 2.5mg, then increased to 5mg and later 7.5mg a week for six months. She became weak and body pains reduced but diarrhoea continued. My brother also a doctor advised to stop Methotrexate. She got some relief from weakness but diarrhoea continued. The stools were gummy brown and green with mixed colour. A general physician suggested colonoscopy. We lost all her previous reports in shifting. The physician told its inflammation. We don't know whether it was reflux esophagytis or not, was given Pantaprazole. She stopped all other medicines. We don't know whether it is candidates or reflux but treatment is Pantaprazole. Biopsy report says it is intestinal tuberculosis. Due to this treatment her body weight decreased. Stools in large volume, mucus without blood. Along with Methotrexate she was given iron syrup Folic acid, B6 and B12.
What is TLC and Mtx Sir?
B6 Because of isoniagid given. The stools were black in colour with blood. Stool test was not done earlier. Gastroenterology surgeon did colonoscopy. Earthere were no black stools. Her ESR was also high.
20-09-2024
PPM 5 - Is the patient conscious and recognising family members?
PA - Yes sir but no hopes.
PPM 5 - Please do not lose hope and be positive when with patient.
PA - She is unable to breath sir. What should we feed her?
PPM 1 - Ask the resident there to share her Respiratory rate and spo2. You can feed Idly or whatever she likes.
RESIDENT - Spo2 on RA 88, RR 40 sir.
PPM 1 - We need to start CPAP but it needs to be a dedicated CPAP machine only to be used in her to prevent transmission of mycobacteria to other potential users.
PA - Sir she removed nebulizer. I will take her home sir. Please remove her ventilator. Is she having TB?
PPM 1 - It's likely to be TB in her lungs but she also needs good care for her diabetes, esophageal candidates and mental health.
PA - OK Sir.
PPM 3 - What happened to her mental health?
PPM 5 - Patient is in depression due to prolonged illness. But was very active when I spoke to her.
PPM 3 - It can also be the other way around. She had physical illness because of mental health.
PA - In 2013 we thought it was irritable Bowel syndrome.
PPM 1 - You had given an appointment there so that you could know exactly what happened to her mental health. I guess they didn't call?
PA - Where should we go to consult him in the evening?
PPM 1 - This will need home health care which @PPM5 is trying to develop in Telangana and Pan India. This means we need resources at her home such as :
HUMAN RESOURCES:
The patient relatives should be able to share her hourly respiratory rate and Spo2 and other issues with our PaJR team here and share her seven point sugar profile either with Glucometer as here or through CGM device.
TECH RESOURCES:
Glucometer, Spo2, BP, ECG monitoring devices and oxygen supply and if possible a non invasive CPAP machine available on rent.
We can send her LAMA on empirical antitubercular therapy and she can have a home drawn weekly blood test for hemogram. LFT, RFT monitoring. We can keep dose titrating her Insulin based on the seven point sugar profile data shared by the PA here .
You just needed to call him yesterday at the time he provided! @PPM6 can you reschedule your appointment and provide them with another time for them to call today?
PA - Not required sir. I will take her home.
PPM 1 - @PPM2, PPM7 please mention this current plan in our LAMA summary.
PPM 2 - OK Sir.
PPM 1 - Today's update before the LAMA.
The Morning respiratory distress and hypoxia necessitating non invasive ventilation appears to have been precipitated by a transient tachypnoeafrom her anxiety? Currently she is much better, sleeping with near normal respiratory rate and normal Spo2.
PPM 1 - She is probably having intermittent MAT due to her lung issues. And the intermittent MAT may have precipitated her transient heart failure issues.
PPM 1 - VITALS and sugar chart post admission.
PPM 5 - Advised patient attendant to speak to palliative care Specialist in Hyderabad to get an advice. 🙏
PPM 1 - From our current assessment her condition is treatable if this is just a Diseminated Tuberculosis. We are trying to convince the patient to stay. @ PPM6 please see if you can provide us with another appointment today.
20-09-2024
PPM 1 -
PARTICIPANT 20- Given the loose stools and the hyponatremia and the unexplained acidosis and the background of TB has adrenal insufficiency been ruled out sir?
How's her BP like?
PPM 7 - BP - 80/40mmhg. PR - 101 b/min
RR - 25 cpm, Spo2 - 85%.
PARTICIPANT 20 - Looks like a distributive adrenal insufficiency?
PPM 7 - Adrenal insufficiency secondary to Adrenal TB?? Sir?
PARTICIPANT 20 - Yes if the suspicion is for diseminated TB .
PPM 1 - Yes it's likely.
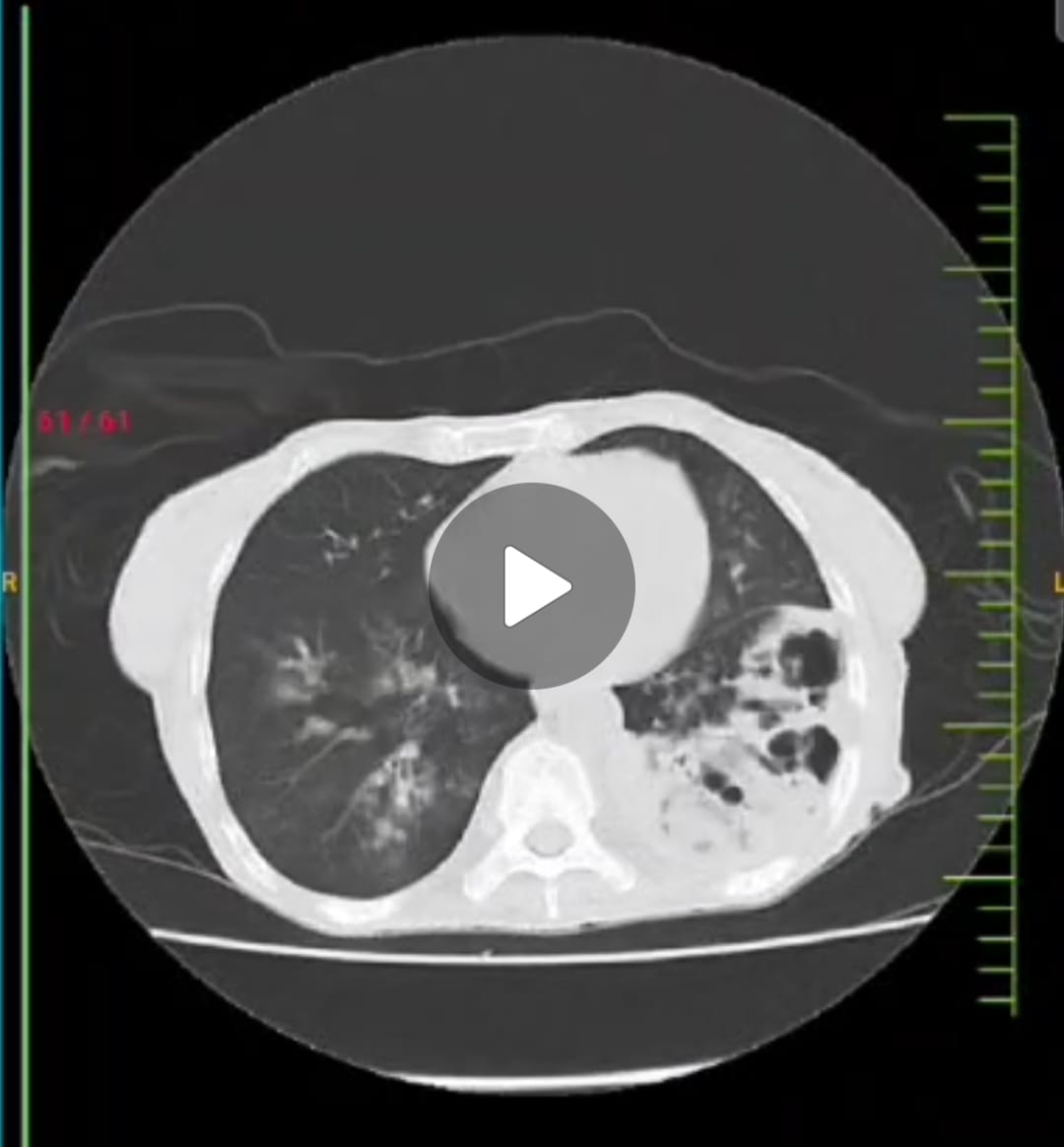
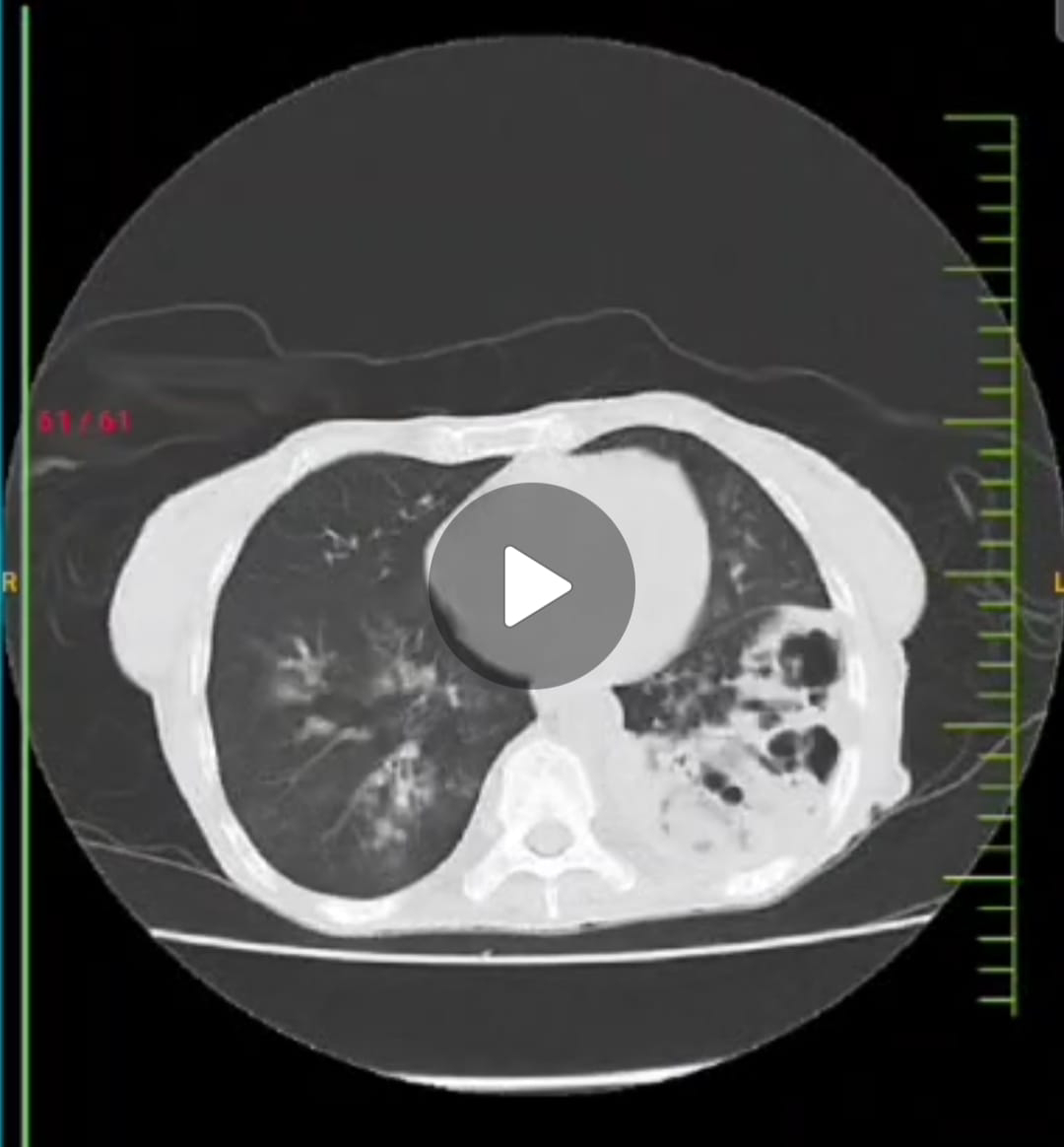
Any update on her current IP status? HRCT Chest?
PPM 7 - Currently admitted. HRCT not yet done sir.
PARTICIPANT 20 - Can do a trial of Hydrocortisone then?
PPM 1 - Agree. Although would be better to cover for mycobacteria first given that there's high chances of MDR.
PARTICIPANT 20 - Absolutely.
PPM 1 - One of the challenges would be breaking up the DOTs supplied tablets to fit her per kg body weight @PPM7 and @PPM2 can you share her current body weight. Someone can lift her and stand on the scales and then deduct his or her body weight.
PPM 7 - @PPM2 is trying by making her stand sir.
PPM 1 - Alright. Yes she did demonstrate an ability to stand without support yesterday, I forgot.
PPM 2 -
PPM 2 - Yes sir.
PPM 1 - Let's calculate the ATT dose now as per kg body weight and then figure out how to break the tablets.
PA- Sir the patient is suffering with cough, please remove her mask. She is requesting sir.
PPM 1 - Remove her mask. I guess it is the CPAP mask?
PA - Yes sir.
PPM 2 - She is on O2 mask only sir till now. Tried convincing for CPAP but not willing. So on O2 mask only.
PARTICIPANT 20 - Has the new regimen of Bedaquiline and Pretomanid for MDR TB kicked in yet nationally?
PA - Thank you sir. I could not take psychologist suggestion at 7pm sir. But I think she needs psychiatrist suggestion.
PPM 7 -
21-09-2024
PA - Sir the stools pic. of the patient. Blood is there with red colour.
Sir the patient's voice is changed sir why?
Tooth discoloration? Fluorosis? She is not brushing her teeth.
PPM 1 -
60F With Multiple lower lobe cavitation lesions with apparent pleural involvement. Thanks for sharing this. Yes there's a possibility that she's loosing blood through her stools as a result of slow GI bleed. Can you share the image of the teeth? Since when was it noticed?
PPM 1 - @PPM7, PPM2, PPM9 Let's try to do an Ultrasound guided left lower pleural aspiration in the morning today ASAP.
PA - No Sir , no discoloration of teeth.
PPM 7 - First sample for occult blood was Negative sir. @PPM10 What happened to yesterday's sample. Was it sent?
PA - From 2days cough is like whoozing cough, gave honey. Sometimes she is having respiratory problems and sometimes needs oxygen mask. Collected the stools again.
PPM 1 - Share the image of yesterday's 24hr sputum collection in the glass.
PA -
PPM 1 - You need to show us whatever is collected in that half filled glass of water in 24hrs and then discard the water in the glass and refill it again next day and again share the image after 24hrs. But it doesn't rule out a lower GI bleed. @PPM2 get a psychiatry consultation today ASAP. Prepare the pleural Fluid aspiration tray and take signed informed consent for both the procedure as well as the case report.
PA - OK Sir from tomorrow.
Sir I came to know that there is a drug sensitivity test before ATT.
PPM 2 - PA Sir, I have been trying to reach you . Psychiatry and ENT people have come to see the patient and they need you for detailed history. Please come to ICU.
PA - I am coming in 10min. At home.
PPM 7 - Spoke to PPM11 and PPM12. Sir told that FNAC wasn't done till now for that type of cavities, and if needed their PGs will guide for USG guided FNAC, and asked to take opinion of pulmonologist and pathologist.
PPM 1 - FNAC is not for the cavity but the pleural infiltration. Yes please always involve the pulmonology and pathology.
PA - The patient is experiencing vomiting sensation and respiratory problem is severe as of now. Nobody told her that the TB drug is being used. But she has vomiting sensation. Sir please confirm whether it is TB or irritable bowel syndrome. We did not tell her about administering TB drugs.
PARTICIPANT 20 - This is an expected and often mild complication with ATT. We can do a liver function test later to rule out hepatitis but the vomiting should settle with some medicines.
PPM 2 -
PPM 1 -
Done in the morning today. @PPM13 Let's start her on the ATT today as calculated in 2 tablets here, @ PPM14 please collect it from the DOTs ASAP.
Let's try to suction out the phlegm currently heard in her throat and send that for Smear and CBNAAT ASAP. We can request the MS and Vice Principal Admin to allow the microbiology to process the sample after duty hours.
PA - Since one year she is having high volume yawning. Why sir?
PPM 1 - It is related to her airway involvement by the infection.
PA - The suction procedure is done. Thank you.
PPM 1 - Also related to the thermo regulatory system.
https://www.researchable.net/publication/26719838-Excessive yawning_ and_thermoregulation_Two_Case histories_of_chronic_debilitating_bouts_of_yawning.
PPM 7 - Given in the morning sir.
PA - After the suction of sputum she is looking bright.
PPM 7 - Spoke to the pathologist. They will plan to do on Monday itseems sir.
PPM 1 - Oh from DOTs. Yes that will help to rule out malignancy even if there's a slightest suspicion.
PPM 7 - Yes sir
22-09-2024
PA - Sir the patient is having pain in the buttocks because of being on the bed for many days. She ate 1 Idly, 50ml milk with protein powder. One spoon honey. Can we give egg white or yellow?
PPM 1 - You can give both, but should be boiled properly to avoid infection.
We can encourage her to walk around from time to time.
PA - Very good line of management. I wish they do RFT, LFT, USG Abdomen and Gynaec examinations too.
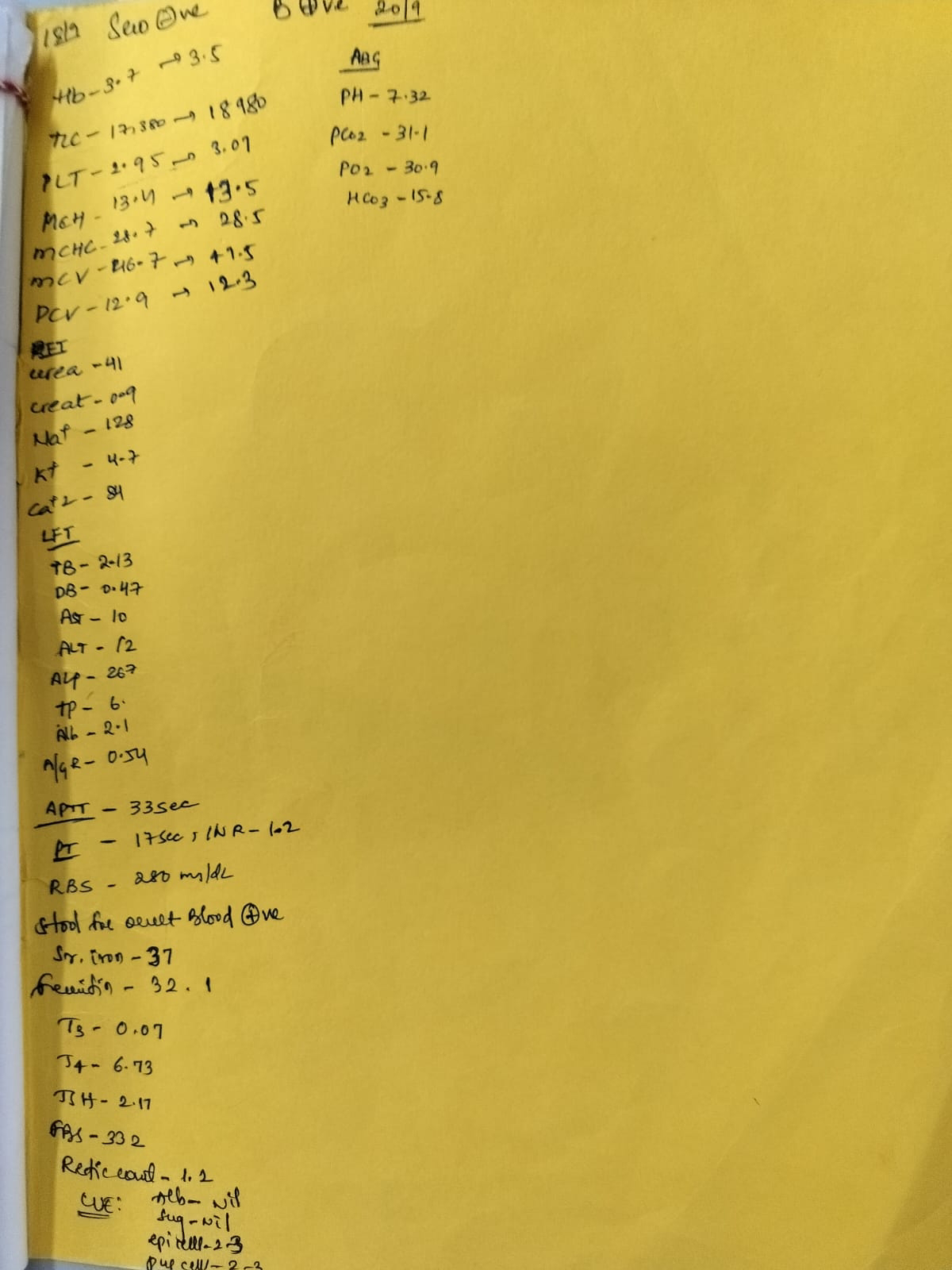
PPM 1 - Here's her LFT and RFT.
23-09-2024
PA - She is unable to flex her knee sir.
PPM 1 - Because of being bedridden for quite sometime. She needs to walk daily.
PA - Can it be cured?
PPM 1 - For her knee issue walking is the best cure.
PA - OK Sir. ATT medicine not available in the pharmacy.
PPM 1 - It's available free of cost from our DOTs Centre downstairs.
PA - Thank you sir. The patient ate one idly and 50ml milk with 1 teaspoon protein powder.
PPM 1 - Yesterday's 24hr urine output was 1ltr @PPM2?
PPM 7 - 1/0 - 1750ml/350ml sir.
PA - Approx 1000ml
PPM 1 - Yesterday's entire day?
PA - Yesterday 12 noon to today 12 noon she passed urine only once , that too today morning only. Urine colour is red(maybe because of ATT)
PPM 1 - AS per sister it's 200ml till @PPM2?
@PPM13 We had planned for the FNAC from the superficial pleural lesion on Saturday alongwith radiology and pathology. Please check what happened with that ASAP
PA - Sputum result has not come yet. Today they are doing FNAC test.
PPM 1 - Yes we did that just now. @PPM2 please ask them to look for AFB.
PPM 2 - OK Sir.
PA - Thank you sir. It's for Carsinoma rule out?
PPM 1 - Just to rule it out. If we are lucky we may even see the TB organism in that slide. What happened to her sputum AFB Smear report @PPM14? Please take another appointment from @PPM6 for her.
24-09-2024
PA - Sir how to take appointment of @PPM3?
PPM 1 - He is in our PaJR group virtually right here @PPM6. He already gave you a telephonic appointment here earlier. He was working in our brick and mortar in our campus before but currently if you want to meet him face to face @PPM5 can manage a brick and mortar appointment with him in Hyderabad.
PA - At present I cannot go to Hyderabad I will telephonically contact him.
PPM 1 - Blood sugar charts of this patient.
PPM 1 - @PPM13 and @PPM2 We can reduce the regular insulin dose before meals or RT feeds.
@PA You can take consent form from our hospital staff.
PA - OK Sir.
25-09-2024
PA - Sir please understand her input also. She is taking only 75ml milk in the morning and 75ml of Ragi malt rarely and either one idly or one egg white. She is unable to eat because of burning sensation in the mouth. 2 yrs back she had the same problem of loss of apetite and side effects. One teaspoon protein powder with milk.
PPM 1 - Yes absolutely. The monitoring has to be both input as well as output.
@PPM2 please share her daily input output since admission that is entered day wise in her fever chart.
PPM 2 - 20-09-2024 - 1850ml/300ml
21-09-2024 - 1500ml/280ml
22-09-2024 - 1050ml/250ml
23-09-2024 - 1750ml/250ml
24-09-2024 - 1750ml/700ml
PPM 1 - 1.7 - 1.8 ltrs are her oral inputs?
PPM 2 - Yes sir both combined with IV + Oral.
PPM 1 - IV everyday? How much IV everyday?
PPM 2 - 1 pint sir.
PPM 1 - Which means yesterday she consumed 1275 ml orally @PA?
PPM 1 - Just let it be 6U NPH twice a day and stop HAI before meals and we can decide on how much HAI to add once we again see how she's doing on 6U NPH twice a day.
PA - What is 1850ml/300ml?
Sir the technician told min 1 ml required for sputum test.
She needs to see the doctor, she is in emergency.
PPM 1 - Yes she had a sudden bout of gasping and had a cardiac arrest from which she could not be revived. I met your son just now in ICU.
26-09-2024
PA - Thank you to all the general medicine department doctors, senior doctors and all the train doctors under him, staff sisters, interns, all helpers of the hospital each and everyone for their exceptional services. Thank you all.
PPM 1 - Thanks.
We shall begin the autopsy after 10am.
EMR SUMMARY
Age/Gender - 60 / Female
Address -
Discharge type - Expired.
Admission Date - 18-09-2024. 7.54pm
Death Date - 25-09-2024.
DIAGNOSIS
Probable MILIARY TB for further investigation confirmation.
K/C/O Intestinal TB 2yrs back.
Drug induced Hepatitis (Resolved)
Oro Pharyngeal Candidiasis, Chronic Diarrhoea?
IBS - D Anemia of Chronic disease - Iron deficiency secondary to upper GI blood loss.
B12 deficiency.
K/C/O HTN, DM II Since 20yrs.
Case History and Clinical Findings.
Chief Complaints
C/O Loose stools and fever since 2 days.
C/O Decreased apetite since 2 days.
HISTORY OF PRESENT ILLNESS
Patient was apparently alright 4 yrs back then she was diagnosed with intestinal TB and started on anti TB drugs used for one and half month and stopped due to deranged LFT and started on second line anti TB drug (Streptomycin) and due to giddiness she again stopped medication. Since 3 yrs she is not on any medication. She lost 5kgs in 4 yrs, decreased apetite since 1 Yr and completely stopped taking food since 2 days. Loose stools since 2 days, large quantity, 5-6 episodes daily, foul smelling, mucoid in consistency. Fever on and off high grade associated with sputum since 2 days.
PAST HISTORY
K/C/O HTN, DM II Since 20yrs.
K/C/O Intestinal TB 4 yrs back.
Surgery for Hernia 10 yrs back.
2 LSCS.
At time of admission:
Temperature - 102°F
BP - 120/50mmgh.
PR - 122 b/min
RR - 25 CPM
SpO2 - 92%
RA GRBS : 262mg/dl
Pallor - Present
Edema of feet - Present.
No Icterus, Cyanosis, Clubbing, Lymphadenopathy.
CVS : S1 S2 +ve.
No murmurs
RS : BAE +ve
NVBS: No added sounds
P/A - Soft non tender
CNS : NFNO.
COURSE IN HOSPITAL
COURSE IN HOSPITAL
A 60yr old female came with complaints of loose stools and fever since 2 days.
C/O decreased apetite since 2 days.
Patient was thoroughly examined and relevant investigations were done. Patient was diagnosed as Desiminated Miliary TB.
K/C/O Intestinal TB 2yrs back, drug induced hepatitis (resolved)
Oro Pharyngeal Candidiasis.
Chronic diarrhoea?
IBS - D
Anemia of Chronic disease- Iron deficiency
Secondary to upper GI blood loss.
B12 deficiency.
K/C/O HTN, DM II Since 20yrs.
During the course patient was treated conservatively with IVF's, antibiotics, antipyretics , antifungal Heamantics, Multivitamins, PPIs and other supportive treatment was given.
During the stay in hospital patient improved clinically and is being discharged in Hemodynamically stable condition.
LAMA NOTES:
Patient condition, prognosis and further plan of treatment in hospital stay has been explained to the patient attenders and patient in their own understandable language. Due to the terminal illness of the patient with poor prognosis and her refusal to take treatment, they want to take her home considering and respect to the patient's autonomy.
Doctor/Hospital management are not responsible for any untoward incidents outside the hospital.
Doctor/Hospital management are not responsible for any untoward incidents outside the hospital.
INVESTIGATIONS
18-09-2024
COMPLETE URINE EXAMINATION (CUE)
Colour - Pale yellow
Appearance - Clear
Reaction - Acidic
SP Gravity - 1.010
Albumin - Nil
Sugar - Nil
Bile Salts - Nil
Bile pigments - Nil
Pus cells - 2-3
Epithelial cells - 2-3
RBC - Nill
Crystals - Nil
Casts - Nil
Amorphous deposits - Absent
Others - Nil
18-09-2024
RFT
Urea - 41mg/dl
Creatinine - 0.9mg/dl
Uric acid - 4.4mm/L
Calcium - 8.4mg/dl
Phosphorus - 2.9mg/dl
Sodium - 128mmol/L
Potassium - 4.7mmol/L
Chloride - 84mmol/L
LFT
Total bilurubin - 2.13mg/dl
Direct bilurubin - 0.47mg/dl
SGOT (AST) - 10IU/L
SGPT(ALT) - 12IU/L
Alkaline phosphatase - 267 IU/L
Total proteins - 6.0mg/dl
Albumin - 2.1gn/dl
A/G Ratio - 0.54
HBSAG - Rapid
Negative Anti HCV antibodies- Rapid
Non reactive HIV
Half Rapid Test - Non reactive
19-09-2024
THYROID PROFILE
T3 - 0.07ng/ml
T4 - 6.73mg/dl
TSH - 2.17 micro IU/ml
STOOL FOR OCCULT BLOOD
Positive (+ve) stool for occult blood
Positive (+ve)
20-09-2024
ABG
PH - 7.32
PCO2 - 31.1
PO2 - 30.9
HCO3 - 16.6
BEB - 9.1
BEECF - 9.0
TCO 2 - 36.402
SAT - 34.602
Count - 1.6
APTT - 33 sec
PT - 17sec
INR - 1.2
BGT - B+
FBS - 332mg/dl
Reticulocyte count - 1.2%
Serum Iron - 37mcg/dl
Serum. Ferritin - 32.1ng/dl
HEMOGRAM DONE ON 18-09-2024
Hemoglobin - 3.7gm/dl
Total Count - 17380 cells/cumm
Neutrophils - 88%
Lymphocytes - 07%
Eosinophils - 00%
Monocytes - 05%
Basophils - 00%
PCV - 12.9 vol%
MCV - 46.7fl
MCH - 13.4pg
MCHC - 28.7%
RDW - CV - 22.3%
RDW - SD - 36.3fl
RBC Count - 2.76 millions/cumm
Platelet Count - 2.95 lakhs/cumm
Smear - Mycrocytic hypochronic Anemia with neutrophilic leucocytosis.
19-09-2024
HEMOGRAM
Hemoglobin - 3.5mg/dl
Total count - 18980 cells/cumm
Neutrophils - 86%
Lymphocytes - 10%
Eosinophils - 00%
Monocytes - 04%
Basophils - 00%
PCV - 12.3vol%
MCV - 47.5fl
MCH - 13.5pg
MCHC - 28.5%
RDW - CV - 22.5%
RDW - SD - 37fl
RBC Count - 2.59 millions/cumm
Platelet Count - 3.07 lakhs/cumm
Smear - Microcytic hypochronic Anemia with neutrophilic Leukocytosis.
18-09-2024
USG ABDOMEN
IMPRESSION
Right grade IRPD changes left small Kidney irregular urinary bladder wall thickening?
Cystitis correlate with CUE.
19-09-2024
2D ECHO
No RWMA paradoxical IVS mild TR: No PAH: Trivial ARI MR Sclerotic AV: No AS/MS IAS Intact.
EF - 64%
Good LV Systolic function Grade 1
Diastolic dysfunction present.
No PE or LV Clot
IVC Size - 0.6 MS Collapsing.
TREATMENT GIVEN
IVF NS @ 30ML/HR Inj.Optineuron 1 amp in100ml NS/ IV/OD
Inj.Neomol IGM IV/ SOS.
Inj.Augmentin 1.2gm IV/TID × D2 .
Tab.Azithromycin 500mg PO/OD × D2
Tab.PCM 500mg PO/SOS
Inj.HAI 6U/SC/TID.
Inj.NPH 4U/SC/BD
Tab.Livogen 150mg PO/OD
Tab.Flucanazole 150mg PO/OD
Candid mouth paint LA/TID
Tab.Becosules. PO/OD
2 Egg Whites per day
Protein powder 2 scoops in 1 glass of water or milk PO/TID
NEBS with Budecort 12th hrly.
Ipravent 8th hrly
Dorolac - z Sachets PO/BD
Death Date - 25-09-2024
Ward : ICU
Unit - III
Faculty Signature:
Signature of patient/Attender:
Signature of PG/Internee :
Signature of Administrator :
Signature of faculty:




















No comments:
Post a Comment