THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE-IDENTIFIED HEALTH DATA SHARED AFTER TAKING HER SIGNED INFORMED CONSENT. HERE WE DISCUSS OUR PATIENTS PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY EXPERTS WITH AN AIM TO SOLVE THOSE PATIENTS CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUTS.
A case of 30 year old female
33 year old female came with the chief complaints of:
1.arthralgia since 2 months
2.fever since 5 days
3.vomitings and loose stools since 4 days
4.abscess over the right thigh (?ruptured)
since 5 days .
HOPI :
Patient was apparently asymptomatic 2 months ago then she developed fever which is of low grade associated with polyarthralgia lasted for 15 days for which she used Tab . Paracetamol ,Tab.Diclofenac after which the patient still didn't get any relief
There's no effect of her symptoms on her daily activities and her occupation.
The patient took COVID vaccine
H/o small and large joint pains with swelling around the joints
Due to the persistence of fever and polyarthralgia the patient visited rheumatologist in the month of October (RF -Normal ,HB - 9 g/dl, ESR -110)
There the patient was advised:
1.Tab. HCQ 200 mg OD for 2 weeks (8pm)
2.Tab.Prednisolone 20 mg OD for 2 weeks (8am)
3.Tab.Azathioprine 50 mg OD in the morning for 2 weeks
After using these medicines her symptoms got subsided
Today patient has come to our hospital with fever which is of high grade associated with chills and rigors , vomitings - non bilious, non-projectile, food and water as the content, stools - watery in consistency, large volume mucous, no blood in stools
No h/o Malena, hematuria
Past history:
Not a k/c/o diabetes mellitus, hypertension, asthma, cad, tuberculosis
Past surgical history:
Tubectomy done 10 years ago
Personal history:
Diet -mixed
Appetite - decreased since 2 months
Bowel habits - regular
Bladder habits - urgency present
Sleep - adequate
No addictions
Family history:
Patient's mother is a known case of diabetes and hypertension since 10 years
Obstetric history:
Age of marriage - 18
P2L2
General examination:
Patient is conscious, coherent,cooperative, thin built and poorly nourished
Mild pallor present
No cyanosis, icterus, clubbing,lymphadenopathy, edema
Mild dehydration present
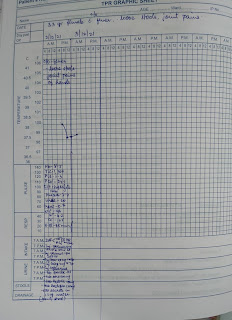
Vitals:
Pulse rate - 88 bpm
Temperature- 100 degree Fahrenheit
RR - 12 cpm
BP - 80/50 mmHg
Systemic examination :
CVS: S1 S2 +, no added murmurs
RS :BAE +, NVBS heard
CNS: no focal neurological deficits
P/A: soft non tender
No organomegaly
No distension
Bowel sounds heard
Local examination of the abscess:
1 x 1 cm wound present over the anterior aspect of left thigh with surrounding erythema.
Local rise of temperature +
Tenderness +
No pus discharge
(Diagnosis given by the surgery dept for the abscess - Ruptured sebaceous cyst)
Advice given for the abscess:
1.Tab CHYMEROL forte -TID
2.Tab Hifenac -P PO /BD
3.Tab Vit -C PO /OD
4.Regular dressings
Investigations sent on the day patient got admitted : (2/12/2021)
1.ECG
2.USG abdomen - no sonological abnormality detected
3.RFT: urea - 20 mg/dl, creatinine - 0.7 mg/dl, Na+ - 146 meq/L, K+ - 4.2 meq/L, Cl- 105 meq/L
4.LFT: TB - 1.21, DB - 0.26, AST - 26, ALT - 10, ALP - 95, TP - 5.9, Albumin - 3.2, A/G ratio - 1.22
5.Hemogram: HB - 8.5 g/dl, TLC - 1,300, N/L/E/M - 61/27/2/10, PLt - 1.19, RBC - 2.90
PCV - 24.1, MCV - 83.1, MCH - 29.3
6.ESR - 85 mm
7.CUE: Sugar, albumin - nil, pus cells - 3 to 4
E.cells - 2 to 3
8.Malarial parasite - negative
9.Chest x-ray
Previous investigations of the patient:
13/9/2021
HB - 9.5 g/dl
TLC - 2,900
PCV - 28.1
PLt - 1.89
K+ - 2.8
23/10/2021:
HB - 9 g/dl
TLC - 4,900
PLt - 2.69
R factor - normal
CRP - 9
ESR - 10
Alb - 3.9
TSH - 7.16 micro IU/ml
USG - free fluid in the pelvis
Provisional diagnosis:
Acute Gastroenteritis (infective cause) with ruptured sebaceous cyst with polyarthralgia under evaluation.
Treatment given:
1.IVF - NS, RL @ 100 ml/hr
2.Inj Optinneuron 1 amp in 100 ml NS IV/OD
3.Inj Neomol 1 gm IV SOS (if temp >=101 degree Fahrenheit)
4.Inj Pantop 40 mg IV OD
5.Inj Zofer 4 mg IV TID
6.Inj Ceftriaxone 1 gm IV BD
7.Tab Sporolac -DS PO TID
8.Tab Dolo 650 mg PO TID
9. Tab Baclofen 12.5 mg PO SOS (if hiccups persist)
10.ORS sachets in 1 litre of water - 100 ml /stool.
11.Tab Redotil 100 mg PO /BD
28 year old married woman, mother of two, from nalgonda , who does maggam work on blouses,
came for follow-up,
patient was apparently asymptomatic till July 2021, when she first developed low grade fever ,which was present daily, increasing during evening time, for which she took tab dolo 650mg everyday for one month, after which she started having joint pains (b/l knee, ankle, elbow, metacarpophalangeal and proximal interphalangeal joints) associated with swelling, with slight restriction of movement for one month.
later she developed oral ulcers, which were painful.
she also had increased hair fall, but no alopecia.
h/o rash over cheeks? photosensitive
h/o pedal edema pitting type upto ankle.
Her first consultation with a physician was in September 2021, where she was adviced to get ana profile done, and was diagnosed with pancytopenia, and started on hcq 200 mg and prednisolone 10 mg twice per day, azathioprine 50 mg which she used for 2 months and discontinued as her joint pains and swelling subsided.
On Jan 1st, she had sudden onset weakness of left upperlimb , which resolved within 6 hours, not a/w seizures, loss of consciousness. She was started on mycofenolate mofetil 1gm/day which was tapered to 500mg od within 2 weeks, (SLEDAI-14) with follow-up every two months.
since Feb 2022 she has been skipping doses of mycofenolatte, due to financial issues and is taking it three times a week.
Personal history: She has a normal appetite, consumes grains, Vegetables, meat, and has resumed her work in blouse designing.
menstrual history:
regular cycles 3-4 days /30, 3 pads per day, no clots, missed period for 2-3 months during fever episodes.
General examination:
built: thin
Skin: no hyperpigmentation currently.
pallor: absent
icterus: absent
cyanosis: absent
clubbing: absent
lymphadenopathy: absent
edema :absent
PR: 96/min ,regular
BP:110/70 mmhg
January 2022
Musculo skeletal examination:
Axial skeleton:
1)Cervical spine: normal
2)Thoracic spine: normal
3) Sacro-iliac joint: normal
Appendicular skeleton:
1)Shoulder joint: no swelling
No tenderness
Range of movements: Normal
2)elbow joint: no swelling
No tenderness
Range of movements: Normal
3)elbow joint: no swelling
No tenderness
Range of movements: Normal
4) wrist joint: normal
5) hand: metacarpophalangeal joint: normal
Interphalangeal joint: normal
6) knee joint:no swelling
No tenderness
Range of movements: Normal
7) ankle joint: no swelling
No tenderness
Range of movements: Normal
8) metatarsophalangeal joint: Normal.
Systemic examination
CNS: conscious
Oriented to time ,place, person
Speech: normal
Memory: intact
Intelligence: normal
Cranial nerves: normal
Sensory system:normal
Motor system: normal.
Cerebellum: normal
CVS: Apex beat in 5th ics ,mid clavicular line
S1 and S2 heard in all areas
R.S: bilateral airway entry present,
normal vesicular breath sounds in all areas
GIT:no oral ulcers currently
no tenderness, free fluid, organomegaly.
Investigations
5/8/21--------------------10/10/21--------may 2022
Hb-7.4 gm/dl. 8.9. 11.7
Tlc-3600 cells/cm3. 3400. 6600
platelets -1.9lakh/cm3. 1.84. 3.3lakh
esr-110mm/hr. 10
crp-9.0. negative
RF-negative
peripheral smear -normocytic, normochromic.
12/12/2021
ana-positive
anti ds dna-strongly positive
anti sm-negative
c3-76.8 mg/dl (low)
c4-normal
As per SLICC criteria (6) in November 2022
clinical-leukopenia, thrombocytopenia,oral ulcers,synovitis
lab criteria-anti dsdna, low complement,
current treatment
tab.mycophenolate mofetil 500mg od
Tab Prednisolone 20mg od
Tab hcq 200 mg od
Tab.Aspirin 75mg od
Final diagnosis: connective tissue disorder, likely systemic lupus erythematous in remission
(SLEDAI=0)
Criteria for remission
SLEDAI
A score of 4 or more is indicative of active disease.Critical appraisal:
Enteric-coated mycophenolate sodium versus azathioprine in patients with active systemic lupus erythematosus: a randomised clinical trial
Ordi-Ros J, et al. Ann Rheum Dis 2017;0:1–8. doi:10.1136/annrheumdis-2016-210882
P-A total of 240 patients were enrolled between May 2010 and December 2013. Of the patients in this intention-to-treat population, 120 were randomised to each treatment group.
Eligible patients were aged ≥18 years, had an SLE according to the revised ACR classification criteria and moderate-to-severe active disease defined as: a SLE Disease Activity Index 2000 (SLEDAI-2K)26 total score ≥6 or at least 1 British Isles Lupus Assessment Group (BILAG) A or 2 BILAG B domain scores at screening.
exclusion criteria were immunosuppres-sant therapy 12 weeks before randomisation; active nephritis or non-lupus-related significant laboratory abnormalities.
I-Eligible patients were randomised (1:1) to receive EC-MPS (target dose: 1440 mg/day) or AZA (target dose: 2 mg/kg, per thiopurine methyltransferase levels (TPMT)) in addition to background oral prednisone and antimalarial agents.
O-The primary efficacy endpoints were the proportion of patients achieving at 3 and 24 months, at least 8 consecutive weeks of clinical remission (CR), defined as a clinical SLEDAI-2K=0.
Primary endpoint Clinical remission rates were higher in the EC-MPS group by month 3 (32.5% (39/120 patients)) compared with the AZA group (19.2% (23/120); percentage difference 13.3% (95% CI 2.3 to 24), p=0.034) and sustained throughout the study to month 24 (71.2% (84/118) vs 48.3% (57/118); percentage difference 22.9% (95% CI 10.4 to 34.4), p<0.001)
Secondary endpoints included: the overall proportion of patients in CR and partial clinical response (PR) (≥50% reduction in the total SLEDAI-2K score with a BILAG C score or better, without new BILAG A/B scores); treatment failure (premature discontinuation necessitated by protocol-prohibited rescue therapy due to worsening or persistent disease activity
BILAG A/B flares were more common in the AZA group (71.7% (86/120 patients)) compared with the EC-MPS group (50% (60/120)) (p<0.001).
In the AZA and EC-MPS groups, 34.2% and 35% patients had 1 disease flare; 21.7% and 13.3% had 2 flares; and 16.7% and 5% had >2 flares, respectively.
Mucocutaneous and renal flares were more frequent in the AZA group (p=0.003 and p=0.031, respectively)
Flares were associated with medication reduction in 38 patients (31.7%) of the AZA group and 29 (24.2%) of the EC-MPS group.
Rates of new BILAG A flares were low, but significantly higher in AZA (21.7% (26/120) vs 8.3% EC-MPS (10/120), p=0.004)
33 years old female with weakness in the left upper limb
- Deviation of mouth to right side
- Weakness of Left Upper Limb on 31/12/2021 at 8:14 am.
History of present illness: She was apparently asymptomatic 4 days ago. Then as she was coming out of her washroom she was unable to use her left upper limb followed by which she developed deviation of mouth to the right side. It was associated with drooling of saliva from the right angle of mouth. She also developed parasthesia over face and left upper limb. Her symptoms are improving gradually. She was initially aphasic but now she is able to speak. She also c/o fine tremors in right hand fingers since morning (on 31/12/21).
She was admitted in KIMS, 1 month back for Acute GE with polyarthralgia with hypoproliferative marrow.
- No c/o headache.
- No c/o nausea.
- No c/o fever.
- No c/o vomitings.
Link to the blog when she was admitted for the first time is given as follows-
https://medcases1.blogspot.com/2021/12/a-case-of-30-year-old-female.html
Past history: She is a k/c/o SLE on medication since 2 months.
Not a k/c/o DM, HTN, TB, BA, Epilepsy, CAD.
Family h/o: K/C/O DM and HTN In mother.
Personal h/o:
Diet -mixed
Appetite - decreased since 2 months
Bowel habits - regular
Bladder habits - regular
Sleep - adequate
No addictions
Obstetric history :
Age of marriage - 18
P2L2
General examination: Patient is conscious, coherent, cooperative, thin built and poorly nourished.
Deviation of mouth to right side.
Nasolabial fold on left side absent
Frowning present.
Mild pallor present.
No icterus, cyanosis, clubbing, lymphadenopathy, Edema.
Vitals:
Pulse rate - 80 bpm
Temperature- 98.2 degree Fahrenheit
RR - 15 cpm
BP - 100/80 mmHg
Systemic examination :
CVS : S1 S2 + , no added murmurs
RS :BAE + ,NVBS heard
P/A :soft , non tender
No organomegaly
No distension
Bowel sounds heard
CNS:
GCS- E4V5M6
EOM- Full
Pupils- B/L dilated, reacting to light
Tone- Rt. Lt.
UL N N
LL N N
Power-
UL 5/5 4/5
LL 5/5 5/5
Reflexes-
B- + +
T- + +
S- + +
K- + +
A- + +
P- Flexor Flexor
Hand grip 100% 30%
Provisional diagnosis-
CVA WITH LEFT UPPER LIMB MONOPARESIS WIYH ACUTE INFARCT IN THE RIGHT PARIETAL LOBE.
SECONDARY TO SLE VASCULITIS.
WITH K/C/O SLE
With K/C/O RUPTURED SEBACEOUS CYST.
Investigations:
On 01/01/2022
Treatment:
1. TAB. ECOSPIRIN 150 mg PO/OD/HS
2. TAB. CLOPIDOGREL 75 mg PO/OD
3. TAB. ATORVASTATIN 40 mg PO/OD/HS
4. INJ. DEXAMETHASONE 8 mg I.V./OD
5. INJ. PANTOP 40 mg IV/OD
6. TAB. HCQ 200 m PO/OD
7. BP/PR/TEMPERATURE MONITORING HOURLY
8. GRBS MONITORING 6th hourly
9. PHYSIOTHERAPY OF LEFT UPPER LIMB
EMR SUMMARY
Age/Gender: 36 Years/Female
Address:
Discharge Type: Relieved
Admission Date: 01/01/2022 04:11 PM
Diagnosis
CVA WITH LEFT UPPER LIMB MONOPARESIS WIYH ACUTE INFARCT IN THE RIGHT PARIETAL LOBE.
SECONDARY TO SLE VASCULITIS. WITH K/C/O SLE
With K/C/O RUPTURED SEBACEOUS CYST.
Case History and Clinical Findings
A 33 years old female came to the GM OPD with chief complaints of
- Deviation of mouth to right side
- Weakness of Left Upper Limb on 31/12/2021 at 8:14 am.
History of present illness: She was apparently asymptomatic 4 days ago. Then as she was coming out of her washroom she was unable to use her left upper limb followed by which she developed deviation of mouth to the right side. It was associated with drooling of saliva from the right angle of mouth. She also developed paraesthesia over face and left upper limb. Her symptoms are improving gradually. She was initially aphasic but now she is able to speak. She also c/o fine tremors in right hand fingers since morning (on 31/12/21).
She was admitted in KIMS, 1 month back for Acute GE with polyarthralgia with hypoproliferative marrow.
- No c/o headache.
- No c/o nausea.
- No c/o fever.
- No c/o vomitings.
Past history: She is a k/c/o SLE on medication since 2 months. Not a k/c/o DM, HTN, TB, BA, Epilepsy, CAD.
Family h/o: K/C/O DM and HTN In mother. Personal h/o:
Diet -mixed
Appetite - decreased since 2 months Bowel habits - regular
Bladder habits - regular Sleep - adequate
No addictions Obstetric history:
Age of marriage - 18 P2L2
General examination: Patient is conscious, coherent, cooperative , thin built and poorly nourished. Deviation of mouth to right side.
Nasolabial fold on left side absent Frowning present.
Mild pallor present.
No icterus, cyanosis, clubbing, lymphadenopathy, Edema. Vitals:
Pulse rate - 80 bpm
Temperature- 98.2 degree Fahrenheit RR - 15 cpm
BP - 100/80 mmHg Systemic examination:
CVS: S1 S2 +, no added murmurs RS: BAE +, NVBS heard
P/A: soft, non-tender No organomegaly No distension
Bowel sounds heard CNS:
GCS- E4V5M6
EOM- Full
Pupils- B/L dilated, reacting to light Tone- Rt. Lt.
UL N N LL N N
Power-
UL 5/5 4/5 LL 5/5 5/5
Reflexes- B- + +
T- + + S- + + K- + + A- + +
P- Flexor Flexor Hand grip 100% 30%
Treatment Given (Enter only Generic Name)
1. TAB. ECOSPIRIN 150 mg PO/OD/HS
2. TAB. CLOPIDOGREL 75 mg PO/OD
3. TAB. ATORVASTATIN 40 mg PO/OD/HS
4. INJ. DEXAMETHASONE 8 mg I.V./OD
5. INJ. PANTOP 40 mg IV/OD
6. TAB. HCQ 200 m PO/OD
7. BP/PR/TEMPERATURE MONITORING HOURLY
8. GRBS MONITORING 6th hourly
9. PHYSIOTHERAPY OF LEFT UPPER LIMB
Advice at Discharge
1. TAB. ASPIRIN 75 MG PO/OD X-1-X - CONTINUE
2. TAB. ATORVAS 40 MG PO/OD/H/S X-X-1 - CONTINUE
3. TAB. HYDROXYCHLOROQUINE 200 MG PO/OD X-X-1 - CONTINUE
4. TAB. PREDNISOLONE 40 MG PO/OD 1-X-X - CONTINUE
5. TAB. PAN 40 MG PO/OD 1-X-X - 5 DAYS
6. PHYSIOTHERAPY OF LEFT UPPER LIMB
Follow Up
REVIEW TO GM OPD AFTER 2 WEEKS/SOS.
When to Obtain Urgent Care
IN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.
Preventive Care
AVOID SELF MEDICATION WITHOUT DOCTORS ADVICE, DONOT MISS MEDICATIONS. In case
of Emergency or to speak to your treating FACULTY or For Appointments, Please Contact: For Treatment Enquiries Patient/Attendent Declaration: - The medicines prescribed and the advice regarding preventive aspects of care ,when and how to obtain urgent care have been explained to me in my own language
SIGNATURE OF PATIENT /ATTENDER SIGNATURE OF PG/INTERNEE SIGNATURE OF ADMINISTRATOR SIGNATURE OF FACULTY
Discharge Date 05/01/2022 Ward: FMW
Unit: 6
[02-04-2025 12.03] PPM 1: Had bicytopenia in the first admission and ever since then the hemogram is normal. On MMF 360 bid reduced from 500 bid.























No comments:
Post a Comment