TITLE:
ASSESSMENT OF SERUM MAGNESIUM AND ITS OUTCOME IN ACUTE ISCHEMIC CEREBROVASCULAR ACCIDENTS.
INTRODUCTION:
Magnesium depletion in the diet is more prevalent than generally expected. In
industrialised and developing countries it remains to be most common nutritional
problems. This may be due to result of current changes in agricultural practices, food
preparation techniques and dietary changes. WHO and other health agencies states that
more than 75 to 80% of people do not consume the recommended daily intake of
magnesium (1)
Magnesium depletion is considered to be most under diagnose electrolyte
abnormality in current medicine. The prevalence of magnesium deficiency in hospital
settings has been found to be 7 to 11 %. 40% of patients deficiency also coexist with other
electrolyte abnormalities. (2)
Magnesium deficiency is more common in alcoholics, young people and people who
receive certain medications. It is associated with hypertension, diabetes, coronary heart
disease, stroke, osteoporosis due to thrombogenic and atherogenic disruption of arterial
and cardiac integrity. (3)
The National institute of Health website publishes, in human body for the correct
metabolic function more than 350 enzymes magnesium is needed. “Magnesium helps in
proper functioning of muscles and nerves maintains a strong immunity against infections,
supports bone integrity and keeps the heart work in regular rhythm It regulates blood sugar
values , keeps the blood pressure in control, has a role in protein synthesis and energy
metabolism. Interest is gaining in role of magnesium in the prevention and treatment
of diabetes, hypertension, cardiac, cerebral disorders”. Thus deficiency is considered to
be epidemic deficiency.(4)
In acute cerebrovascular accidents, there occurs a rapid loss of brain magnesium and
potassium levels with rapid uptake of sodium and calcium channels, the lower the
magnesium and potassium concentrations the greater the magnitude of cerebral arterial
contraction.
Interruption of cerebral blood flow will lead on to ischemic cell death causing ATP
depletion and ischemic depolarisation leading to excessive calcium entry which causes
vasospasm.
Cerebral blood flow interruption causes release of excitatory glutamate through NMDA
receptors, which causes influx of calcium and sodium leading onto production of free
radicals and initiation of inflammatory response.
Magnesium exerts neuroprotection in the following ways:
1. It‟s a natures physiologic calcium blocker antagonises calcium mediated metabolic
process.
2. It decreases the release of excitatory neurotransmitter
3. It increases the release of inbitory neurotransmitter
4. It relaxes vascular smooth muscle
5. It decreases platelet aggregation.
AIMS AND OBJECTIVES OF THE STUDY:
AIM OF THE STUDY:
To Study serum Magnesium and outcome of patients In Acute ischemic cerebrovascular
accidents.
OBJECTIVES OF STUDY:
1. To detect the serum magnesium levels in patients of Acute ischemic cerebrovascular
Accidents.
2. To detect the outcome ofacute ischemic stroke patients in accordancewith the
magnesium levels.
VARIABLES MEASURED IN STUDY:
MODIFIED RANKIN SCALE:
The Rankin scale is named after the Scottish physician JohnRankin who made this
scale in view to access the disability of thepatient with specific reference to morbidity
of the patient. The scalewas made to access the patient who suffered from stroke to access
the global disability of these patients was later to be used in clinicaltrail and the name
Modified Rankin scale (mRs).
The Modified Rankin scale was used initially in a study in Great Britain for patients suffering
from TIA. After this the scale has gained popularity and now it is widely used to access the
functional outcomes of patients who suffer from stroke.
Advantages of MRS scale:
1.Easy to perform
2. Takes about five minutes to perform
3. It has close correlation with other stroke scale like the NIHSS scale and theBI
4. The volume of infarct correlates well with the imaging findings of patients with
CVA
5. It has six point score which correlates well with the outcome of patients
6. As in the case of NIHSS there are various mobile phone apps, DVDs, online
certificate courses for Learning the scale
Limitations of the MRS scale:
1. As there are only six point score it is less probable to change than other stroke
scales
2. The specificity of the scale is less
3. Inter observer variability is high with respect to this scale
4. Detailed training in scripted interviews is required to improve the reliability and the
consistency of the scale
PATIENTS AND METHODS:
Methods and study design:
This was a observationl study, done in patients admitted in medical wards of Kamineni
institute of medical sciences, Narketpally, Nalgonda, conducted from October 2018 to September 2020. The study will be approved by the ethical Committee of Kamineni
Institute of medical sciences, Narketpally.
INCLUSION CRITERIA:
1. Diagnosis of ischemic stroke based on history , physical. examination and initial
CT/ MRI of Brain or delayed
CT /MRI scan of brain where first scans were normal.
2. Age greater than 40 years
3. Cerebrovascular accidents occurring less than 72 hours.
EXCLUSION CRITERIA:
4. Chronic kidney disease
5. Alcoholic liver disease
6. Thyroid disorders – hypo/hyperthyroidism
7. Chronic diarrhea
8. Patients on drugs that affect serum magnesium levels like diuretics, digoxin and
drugs like amphotericin B
aminoglycosides
9. Age less than 40 years.
DATA COLLECTION AND METHODS:
patients who have got admitted in medicine ward, in the Institute of Kamineni institute of medical sciences, Narketpally, Nalgonda in Department of General medicine, an observational study was conducted on acute cerebrovascular accident patients for a period of two years. Patients selected for clinical study as per inclusion and exclusion criteria. Informed consent was obtained from the relatives of the cases. Detailed history taking and clinical examination was done. Around 2ml of venous blood was collected from the patients. Blood was allowed to clot and serum was separated by centrifugation. Serum levels of Magnesium were estimated using calorimetric method. Neurological status of the patients suffering from cerebrovascular accidents was assessed at the time of admission and at the time of discharge was assessed using modified Rankin Scale(mRS) and Glasgow coma scale.
STATISTICAL METHODS:
Present study results were obtained by using SPSS statistics 20.0 software, following statistical methods are used in this study:
1. MEAN: It is simplest measure of central tendency and is the arithmetic average of observations.
For a ungrounded data, mean is calculated by
MEAN: Sum of all observations
Number of observations
X = ∑X
n
For grouped data, mean is calculated by
X = ∑ fx
n
Where f is the frequency
x is mid point of class interval
n is total number of observations
2. STANDARD DEVIATION: It is a measure of the magnitude of the variation
present in set of data. It is known as root mean square deviation because it is square
root of the mean of squared deviations from arithmetic mean. It is a summary
measure of the differences of each observation from mean of all the observations.
S = d2
(n-1)
3. Level of significance: The magnitude of risk of making a wrong conclusion of rejecting the null hypothesis that the two groups are from same population is fixed in terms of probability level „p‟ and is known as level of significance.
LINK TO COMPLETE THESIS WITH MASTER CHART:
MASTER CHART
HALL TICKET NO: 18100006002
CASE PRESENTATIONS
LONG CASE;
A 70 years old female patient residing in Nalgonda, is a homemaker, presented to OPD with complaints of- loss of appetite since one week,
- generalised weakness since one week
- fever since 5 days
-burning micturition since 5days
History of present illness-
Patient was apparently asymptomatic one week back then she gradually developed loss of appetite since one week which was not associated with nausea, vomiting, associated with generalised weakness fever since 5 days which was high grade associated with chills and rigors, no diurnal variation, relived on taking medication, not associated with headache, cold, cough. She also started experiencing burning micturition since 5 days associated with low backache, no history of dark coloured urine or blood in urine
no h/o cold, cough, chest pain, palpitations, shortness of breath, pedal edema, reduction in urine output, diarrhoea, constipation, vomiting, nausea, pain abdomen
Past history:
she has been having similar episodes since 2016
she had 1st episode in 2016 it started with fever which was high grade associated with chills and rigors, associated with loss of appetite which were followed by loss of consciousness. she was immediately rushed to a local hospital where the attenders were told that she had high blood pressure and had high blood sugars. she was diagnosed with UTI and was treated with parenteral antibiotics for 5 days and was discharged on oral antibiotics which she took for one week. since then she had been having recurrent episodes of UTI 2-3times every year. after the 2nd or 3rd episode she started having urinary incontinence for which she consulted a urologist and was said to have weakness of pelvic floor muscles and was advised pelvic floor muscle strengthening exercises.
28 years back she underwent hystrectomy
25 years back she had complaints of generalised weakness
↓
went to a diagnostic center and got few investigations done
↓
consulted a physician and was diagnosed with type 2 diabetes mellitus and was started on OHAs
she did not take OHAs regularly
During that time she was residing in Saudi Arabia and her husband took her to regular check ups almost every weekend during that period he sugars were under control with OHAs
↓
In 2007 they moved back to India in 2010 she had uncontrolled blood sugars for which she was started on insulin, she started using insulin pen
↓
In 2013 she consulted an endocrinologist and was started on injections Humalog (insulin Lispro) 28 units in the morning and Basalog (insulin Glargine) 20 units at night
↓
started having tremors, weakness, excessive sweating, and excessive hunger (had recurrent hypoglycemic attacks) during which he son Dental surgeon advised her to reduce the dose of Insulin lispro to 20 units
↓
reviewed with the same endocrinologist and was advised to stop Insulin glargine and was told to take insulin lispro in the evening also
↓
had recurrent episodes of UTI and got hospitalised for the same
↓
10 years back she had chest pain for which she was taken to a cardiologist and was diagnosed with angina and was started on antiplatelets, statins and isisorbide dinitrate (SOS), tab febuxostat 40mg (for joint pains), vitamin D3 supplementation, and was also advised tab nitrofurantoin for 20 days since then she was on a regular follow up with the cardiologist every 3 months
She also started having complaints of tingling and numbness in her lower lower limbs and was diagnosed with peripheral neuropathy secondary to diabetes mellitus and was startedon tab. neuroprime plus (alpha lipoic acid, thiamine, mecobalamin, elemental chromium)
was also diagnosed with CKD and anemia
↓
Diagnosed with Hypothyroidism 5 years back and was started on tab. levothyroxine 50 mcg daily before breakfast
↓
blood sugars were not under control in 2020 consulted an endocrinologist was started on sitagliptin 50mg and metformin 1000mg everyday morning before break
↓
in 2020 she was treated at home by her son for the similar episodes
↓
in 2021 march she had complaints of fever, cough and was diagnosed with COVID 19 infection and was hospitalized
there she was treated with Injection remdesivir for 5 days along with parenteral steroids and was later discharged on oral prednisolone and was gradually tapered over 10 days and then stopped
↓
In July she again had another episode of UTI and was again hospitalized
↓
was brought to our center
Personal history: married with 8 children - 4 sons and 4 daughters all are well at present,
no addictions - non smoker non alcoholic
sedentary habit
adequate sleep
no bowel abnormalities
family history- not significant
treatment history:
used insulin lispro (50%) + insulin lispro protamine 25 units in the morning and evening subcutaneously
used - Tab Ecospirin AV 75/10 mg H/S
tab Met -XL initially 25 mg for few years then 5o mg once daily
tab. feburic acid 40mg
tab tenegliptin 20mg then changed to tab sitaglipten 50mg + metformin 1000mg once daily
vitamin D3supplementation
used multiple antibiotics for recurrent UTI- nitrofurantoin, clarithromycin, piptaz, meropenem, levofloxacin
tab isosorbide dinitrate SOS
PROVISIONAL DIAGNOSIS:
A 70 years old lady with Recurrent complicated UTIs with peripheral neuropathy, secondary to diabetes mellitus (type 2) with hypertension with hypothyroidism known case of ischaemic heart disease.
GENERAL EXAMINATION:
patient is conscious, coherent, cooperative and oriented to time, place and person
patient is lying comfortably in supine position
patient is obese and well nourished
Height- 151 cms
Weight - 57 kgs
BMI - 25.0 kg/m2
face- wrinkled
eye- no abnormalities, baggy lower eyelids, pallor present, no xanthelasma or xanthomas
no cyanosis
oral cavity- lost all teeth, mucosa appears normal
nails- normal, no clubbing
no thyroid enlargement
no lymphadenopathy
neck veins- not distended
skin- normal, No pigmentation, No scars, No atrophic changes
pulse- 110 beats per minute in supine position in right radial artery, regular rhythm, high volume, vessel is thickened, all other peripheral pulses are felt and are normal
BP: 110/80 mmHg in Right arm in supine position
100/80 mmHg in standing position
Respiration-- 20 breaths per min, thoraco-abdominal type
temperature- normal at the time of examination
feet-no pedal edema, no ulcers or calluses
GENITOURINARY SYSTEM EXAMINATION:
per abdomen- no abnormalities, no visible scars and sinuses
foleys catheter is insitu and is connected to urobag
no renal lump felt
renal angle- no tenderness
urinary bladder- empty
local examination - pubic hair-sparse distribution
labia majora, minora- atrophied
external uretheral meatus- no discharge, healthy
per vaginal examination bimanual examination
bilateral fornices free, non tender
anterior fossa normal
posterior fossa normal
Vault intact - no palpable masses felt, no tenderness
NERVOUS SYSTEM EXAMINATION
patient is conscious, cooperative, alert and oriented to time place and person
cranium and spine -normal, no abnormalities
speech- normal
Recent and remote memory intact
1. CRANIAL NERVES
CRANIAL NERVE | TEST | RIGHT | LEFT |
I | Sense of smell i) Coffee ii) Asafoetida | + + | + + |
II | i) Visual acuity – Snellens Chart ii) Field of vision – Confrontation test iii) Colour vision – Ishihara chart iv) Fundus | 6/6 Normal Normal Normal | 6/6 Normal Normal Normal |
III, IV, VI | i) Extra-ocular movements ii) Pupil – Size iii) Direct Light Reflex iv) Consensual Light Reflex v) Accommodation Reflex vi) Ptosis vii) Nystagmus viii) Horners syndrome | full 4mm Present Present Present Absent Absent No | full 4mm Present Present Present Absent Absent No |
V | i) Sensory -over face and buccal mucosa ii) Motor – masseter, temporalis, pterygoids iii) Reflex a. Corneal Reflex b. Conjunctival Reflex c. Jaw jerk | Normal Normal Present Present Present | Normal Normal Present Present Present |
VII | i) Motor – nasolabial fold hyeracusis occipitofrontalis orbicularis oculi orbicularis oris buccinator platysma ii) Sensory – Taste of anterior 2/3rds of tongue(salt/sweet) Sensation over tragus iii) Reflex – Corneal Conjunctival iv) Secretomotor – Moistness of the eyes/tongue and buccal mucosa | Present Absent Good Good Good Good Good Normal Normal Present Present Normal | Present Absent Good Good Good Good Good Normal Normal Present Present Normal |
VIII | i) Rinnes Test ii) Webers Test iii) Nystagmus | Positive Not lateralised Absent | Positive Absent |
IX, X | i) Uvula, Palatal arches, and movements ii) Gag reflex iii) Palatal reflex | Centrally placed and symmetrical
Present present |
|
X1 | i) trapezius ii) sternocleidomastoid | Good Good | Good Good |
XII | i) Tone ii) Wasting iii) Fibrillation iv) Tongue Protrusion to the midline and either side | Normal No No Normal | Normal No No Normal |
MOTOR SYSTEM:
Right. Left
Bulk: inspection UL normal normal
LL normal normal
palpation. UL Normal normal
LL normal normal
Tone: UL normal. Normal
LL. normal. normal
Power UL. 5/5. 5/5
LL: 5/5 5/5
Reflexes.
Superficial reflexes
Right. Left
Corneal. P P
Conjunctival P. P
Abdominal. + +
Plantar flexor flexor
Deep tendon reflexes
Right. Left
Biceps jerk. + +
Triceps jerk . + +
Supinator jerk. + +
Knee jerk + lost
Ankle jerk lost lost
SENSORY SYSTEM
RIGHT. LEFT
SPINOTHALAMIC
crude touch. UL lost in distal parts on both sides
LL lost in distal parts on both sides
pain. UL- lost in distal parts on both sides
LL- lost in distal parts on both sides
temperature. lost in distal parts on both sides in both limbs
post:
fine touch. lost in distal parts on both sides in both limbs
vibration. lost in distal parts on both sides in both limbs
position sensor. lost in distal parts on both sides in both limbs
cortical
2 point discrimination and tactile localization- could not be assessed
CEREBELLUM
titubation - absent
ataxia - absent
coordination- normal
no nystagmus
Romberg's sign could not be checked as patient was feeling weak
NO SIGNS OF MENINGEAL IRRITATION
AUTONOMIC FUNCTIONS:
positional tachycardia- absent
no orthostatic hypotension
sweating- normal
gait: could not be assessed as she was feeling weak
Investigations
FINAL DIAGNOSIS:
1. Recurrent complicated urinary tract infections
2. Complicated Fungal UTI
3. Asymmetric Peripheral neuropathy secondary to Diabetes mellitus type 2
4. Diabetic nephropathy
5. known case of Ischaemic heart disease, Hypertension, Hypothyroidism
SHORT CASE- 1:
A 43 old male patient resident of Nalgonda, farmer by occupation, presented to casualty with complaints of:
Low grade Fever since 1 year.
Cough with sputum since 1 year
Complaints of neck pain since 6 months
Weakness of all both lower limbs since 6 months.
HOPI:
Patient was married at age of 25 and have 3 children, one son and two daughters. He is farmer by occupation. He is occasional alcoholic and chronic smoker (1-2 packs/day) since 20 years. He was apparently alright till 33 years of age, then in view of generalised weakness pt went for routine evaluation and got diagnosed with diabetes mellites- type 2 and is using OHA since 10 years. He takes his medication regularly.
Patient had history of fever since 1 year which was low grade not associated with chills and rigors, intermittent, associated with diurnal variation and night sweats.
He also complains of cough with scanty white color, mucoid expectorant since 1 year, non foul smelling, non blood tinged. No diurnal variation of cough and no chest pain.
He went to local rmp and got symptomatic treatment.
He later developed neck pain, which was sudden in onset gradually progressive. No history of trauma. No radiation.
He then developed weakness of both lower limbs which was insidious in onset, gradually progressive in nature over 6 months. He had difficulty in standing and walking. No history of upper limb weakness.
H/o difficulty in standing from sitting position present.
H/o difficulty in climbing stairs present.
H/o slippage of chappal while walking without knowledge
H/o difficulty in sqatting present .
No h/o difficulty in getting up from lying down.
no h/o difficulty in holding pen/buttoning/unbuttoning
no h/o difficulty in breathing
no h/o difficulty in lifting the head off the pillow
no h/o difficulty to roll over the bed
no h/o involuntary movements.
no h/o fasciculations/muscle twitchings .
h/o sensory deficit in feeling clothes present.
H/o loss of hot/cold sensations present.
H/o tingling and numbness in UL & LL present.
H/O band like sensation present.
H/o cotton wool sensations present.
no h/o low backache
no h/o trauma
no h/o giddiness while washing face
no h/o urgency/hesitancy/increased frequency of urine
no h/o urinary incontinence
h/o fever/
No h/o nausea/ vomiting/diarrhea
no h/o seizures
no h/o spine disturbances
no h/o head trauma
no h/o loss of memory
no h/o abnormality in perception of smell
no h/o blurring of vision
no h/o double vision/difficulty in eye movements
no h/o abnormal sensation of face
no h/o difficulty in chewing food
no h/o difficulty in closing eyes
no h/o drooling of saliva
no h/o giddiness/swaying
no h/o difficulty in swallowing
no h/o dysphagia/dysphasia
no h/o tongue deviation
no h/o difficulty in reaching objects
no h/o tremors/tongue fasciculations
no h/o incoordination or difficulty in performing task
no h/o fever/neck stiffness
no h/o loss of consciousness and involuntary movements, no h/o irrelevant talk, no slurring of speech, no h/o memory loss and hallucinations .no sleep disturbances.
Past history:
No h/o similar complaints in past.
K/C/O DM-2 since 10 years on Glimi -m1 tablet.
Not a known case of HTN/EPILEPSY/CVA/CAD/TB
FAMILY HISTORY - NOT SIGNIFICANT.
SURGICAL HISOTRY - No previous surgeries or blood transfusions.
Personal history:
Mixed diet with normal appetite and normal bowel/bladder movements
H/o alcohol consumption since 90ml weekly twice since 20 years.
H/o smoking (1-2 packs per day) since 20 years.
Summary:
Insidious, progressive bilateral lower limb weakness with paresthesia.
General Examination:
He is a thin built man, who was conscious, coherent
PR of 80bpm, regular rhythm, normovolemic .
Bp - 110/80mmhg
Temp - 98.3 F
SpO2 - 99%
RR - 22 cpm
GRBS - 120 mg/dl.
Head to toe examination:
Hair - Black, thick, non-easily pluckable. No lesions over the scalp.
Eyes - No pallor, no icterus.
General head & neck examination - No abnormalities. No lymphadenopathy.
Axial- Tenderness over cervical spine +
Fingers & Nails - Clubbing +
Lower limbs - No pedal edema.
No neuro -cutaneous markers noted.
CNS EXAMINATION:
HMF-
Patient conscious, co -operative, coherent.
Oriented to place/time/person
no h/o aphasia/dysarthria
no h/o dysphonia
Recent and remote memory intact.
no h/o emotional lability.
1. CRANIAL NERVES
CRANIAL NERVE | TEST | RIGHT | LEFT |
I | Sense of smell i) Coffee ii) Asafoetida | + + | + + |
II | i) Visual acuity – Snellens Chart ii) Field of vision – Confrontation test iii) Colour vision – Ishihara chart iv) Fundus | 6/6 Normal Normal Normal | 6/6 Normal Normal Normal |
III, IV, VI | i) Extra-ocular movements ii) Pupil – Size iii) Direct Light Reflex iv) Consensual Light Reflex v) Accommodation Reflex vi) Ptosis vii) Nystagmus viii) Horners syndrome | full 4mm Present Present Present Absent Absent No | full 4mm Present Present Present Absent Absent No |
V | i) Sensory -over face and buccal mucosa ii) Motor – masseter, temporalis, pterygoids iii) Reflex a. Corneal Reflex b. Conjunctival Reflex c. Jaw jerk | Normal Normal Present Present Present | Normal Normal Present Present Present |
VII | i) Motor – nasolabial fold hyeracusis occipitofrontalis orbicularis oculi orbicularis oris buccinator platysma ii) Sensory – Taste of anterior 2/3rds of tongue(salt/sweet) Sensation over tragus iii) Reflex – Corneal Conjunctival iv) Secretomotor – Moistness of the eyes/tongue and buccal mucosa | Present Absent Good Good Good Good Good Normal Normal Present Present Normal | Present Absent Good Good Good Good Good Normal Normal Present Present Normal |
VIII | i) Rinnes Test ii) Webers Test iii) Nystagmus | Positive Not lateralised Absent | Positive Absent |
IX, X | i) Uvula, Palatal arches, and movements ii) Gag reflex iii) Palatal reflex | Centrally placed and symmetrical Present Present | Present Present |
X1 | i) trapezius ii) sternocleidomastoid | Good Good | Good Good |
XII | i) Tone ii) Wasting iii) Fibrillation iv) Tongue Protrusion to the midline and either side | Normal No No Normal | Normal No No Normal |
MOTOR SYSTEM :
Right. Left
Bulk: inspection normal. Normal
palpation. Normal. Normal
Measurements U/l 28cm. 28cm
L/L 37cm. 37 cm
Tone: UL hypertonia hypertonia
LL. hypertonia. hypertonia
Power UL. 4/5. 4/5
LL:
iliopsoas 3/5. 3/5
adductor femoris 3/5. 3/5
gluteus medius 3/5. 3/5
gluteus maximus 3/5. 3/5
hamstrings 3/5. 3/5
quadriceps femoris 3/5. 3/5
tibialis anterior. 3/5. 3/5
tibialis posterior. 3/5. 3/5
peroneii. 3/5. 3/5
gastronemius. 3/5. 3/5
extensor -
digitorum longus. 2/5. 2/5
flexor digitorum longus 2/5. 2/5
Reflexes.
Superficial reflexes
Right. Left
Corneal. P P
Conjunctival P. P
Abdominal. + +
Plantar EXTENSOR EXTENSOR
cremasteric. + +
Deep tendon reflexes
Right. Left
Biceps. +3 +3
Triceps. +3 ++3
Supinator. +3 ++3
Knee +3 +3
Ankle. +3 +3
Clonus - both knee and ankle present
SENSORY SYSTEM
RIGHT. LEFT
SPINOTHALAMIC
crude touch. N. N
pain. UL- N N
LL- - -
temperature. - -
post:
fine touch. - -
vibration. - -
position sensor. - -
cortical
2 point discrimination - -
tactile localisation. - -
CEREBELLUM
titubation - absent
ataxia - absent
hypertonia. present present
Rombergs sign-
Respiratory system examination:
Inspection
Rt supraclavicular hollowness
Movements of chest appears to be reduced on right side in supraclavicular region
Palpation vocal fremitus decreased in rt supraclavicular area
Percussion
Dull note in rt supraclavicular and suprascapular region
Auscultation
Wheeze in bilateral lung fields on presentation
Crepitations in left infra axillary area and left infrascapular area.
CARDIO VASCULAR SYSTEM: S1S2 heard.
No murmurs. No palpable heart sounds.
PER ABDOMEN -
SOFT, NO ORGANOMEGALY.
NO GUARDING AND RIGIDITY.
BOWEL SOUNDS PRESENT.
INVESTIGATIONS:
Hemoglobin - 12g/dl
TLC - 10,600 cells/cumm
Platelets - 2.90 Lakhs/cumm
Peripheral smear - Normocytic Normochromic blood picture
ESR - 60mm in 1st hour
HBsAg, HIV, HCV - Negative
RBS - 112 mg/dl
Blood Urea - 43 mg/dl
Serum creatinine - 1 mg/dl
Serum Potassium - 4.1 mg/dl
Serum Sodium - 138 mg/dl
Serum Chloride - 100 mg/dl
Complete Urine Examination - No abnormalities
Sputum for Culture & Sensitivity:
Gram stain, Direct smear: Plenty of inflammatory cells (more than 20/hpf). Few epithelial cells, 1-2/hpf.
Plenty of gram positive cocci in pairs in short chains seen.
Impression- Normal flora grown.
FINAL DIAGNOSIS:
CHRONIC BILATERAL SYMMETRICAL MOTOR SENSORY BOTH PROXIMAL AND DISTAL MUSCLE WEAKNESS SECONDARY TO CERVICAL CORD COMPRESSION AT C4 C5 SECONDARY TO TUBERCULOSIS
K/c/o - DM -2
SHORT CASE- 2:
35 year old man working as a food caterer presented to our OPD with the chief complains of Dyspnea at rest since 5 day
Cough with expectoration since 5 days
Bilateral pedal edema since 4 days
Abdominal distension since 3 days
He was a regular alcoholic since the past 10 years and an occasional smoker. He apparently was completely alright until one morning in November 2019 when he had high fever with chills and visited a local hospital where he got admitted, he says the fever was intermittent and more at nights and was often followed by sweating and was diagnosed with malaria for which he received treatment.
In Dec 2019, the following month, he says he started feeling breathless while climbing up the stairs which progressed over the next 5 days to such an extent that he even felt dyspneic even at rest and had dry cough on and off. He says that his dyspnea and cough aggravated on lying in bed. He gradually developed bilateral pedal edema followed by abdominal distension over the next few days which alarmed him and he decided to pay a visit to a doctor. He visited a local hospital and was put on some medications (no documentation) which patient couldn't recall of. Since it did not improve his symptoms he visited our hospital in January 2020.
He however gave no complaints of palpitations, nausea, vomiting, profuse sweating.
He also gave no complaints of reduced urine output, hematuria, frothy urine.
No complaints of burning micturition, diarrhea, vomiting, pain abdomen.
PAST HISTORY:
Since the past 10 years he has been consuming around 180 ml of whiskey everyday. He also tells that he would occasionally smoke cigarette once in a while along with his friends. In those 10 years he never paid a visit to his hometown due to financial issues and decided not to get married anytime soon as he wanted to settle the financial issues his family was facing.
Not a known case of Diabetes, Hypertension, Also no history of CAD, CVA, Bronchial Asthma, Pulmonary Koch's.
PERSONAL HISTORY:
Patient was born and brought up in ***. He was born to a farmer and a housewife. He has 2 elder siblings, his elder sister is married to an advocate and has 2 children and his elder brother is working as a software engineer. He pursued his degree in electronics but was not successful in finding a job in this branch, so he moved to another state 10 years back and started working in a food catering business along with his friends. During his stay outside his hometown, he says he used to often feel lonely and used to often consume whiskey along with his friends which got to a point that he started consuming around 180 ml of whiskey everyday and would occasionally also smoke cigarettes.
He has been having disturbed sleep because of the financial issues his family has been facing. His appetite has increased and more often consumes outside food.
Since the past 10 years he has been consuming around 180 ml of whiskey everyday. He also tells that he would occasionally smoke cigarette once in a while along with his friends. In those 10 years he never paid a visit to his hometown due to financial issues and decided not to get married anytime soon as he wanted to settle the financial issues his family was facing.
On presentation to our hospital:
He was obese with central obesity
His pulse rate was 100 bpm
Blood pressure - 110/70mmhg
RR - 21 cpm
Spo2 - 98% on Room Air
Temp - 98.6 %
GRBS - 151 mg/dl
GENERAL EXAMINATION:
He weighed 98 kgs and his abdominal girth measured 100 cm
He had no pallor, icterus, clubbing, cyanosis, lymphadenopathy
He had bilateral pitting type of pedal edema present upto his knees
JVP was raised
SYSTEMIC EXAMINATION:
CARDIOVASCULAR:
Inspection:
Shape of the chest - Ellipsoid
No dilated veins, scars, sinuses
No cutaneous lesions
No breast abnormalities
Palpation:
Apex beat palpated in 6th ICS 1 cm lateral to MCL
No palpable pulsations in aortic or pulmonary area or tricuspid area
No palpable pulsation
No palpable epigastric pulsations
No palpable pulsations in sternoclavicular area
Auscultation:
Muffled S1, S2 +
RESPIRATORY SYSTEM EXAMINATION:
Inspiratory crepitations in Bilateral in IAA, ISA
PER ABDOMEN:
soft
Non tender
No organomegaly
Bowel sounds +
CENTRAL NERVOUS SYSTEM EXAMINATION:
Normal
PROVISIONAL DIAGNOSIS:
HEART FAILURE SECONDARY TO
? VIRAL MYOCARDITIS
? ALCOHOLIC
REPORTS:
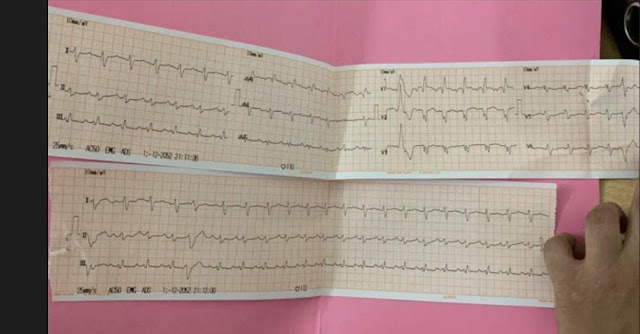
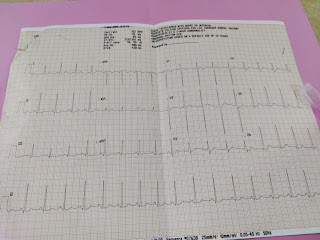
ECG:
His blood picture, renal and liver parameters were in within the normal range.
On routine investigations his HbA1c was found to be 8.4 %.
His Ultrasonography of abdomen revealed Grade 1 fatty liver (probably secondary to his alcohol intake), mild ascites, right moderate pleural effusion.
2DEcho was done which revealed that all the 4 chambers to be dilated with an ejection fraction of 27, global hypokinesia, severe MR, trivial AR, severe LV dysfunction with mild PAH, dilated IVC (2.3cm)
A diagnosis of HEART FAILURE WITH REDUCED EJECTION FRACTION - 27%
DENOVO DETECTED TYPE 2 DIABETES MELLITUS
TREAMENT ADVISED:
He was started on
1. Tab Lasix 80mg in the morning, 40mg in the afternoon and evening
2. Tab Isosorbide mononitrate 10mg twice a day
3. Tab Hydralazine 25mg
4. Tab Telma 40mg
5.Tab Metformin 500mg once a day
and was advised for fluid of less than 1 litre and salt restriction of less than 2grams/day
He was advised for a coronary angiogram for which he visited Hyderabad. CAG was performed on 24th of January 2020 which turned out to be normal and he was started on Tab Vymada 50mg and Tab Met XL 12.5mg
(Sacubitril 26 mg and Valsartan 24 mg) along with Tab Ecosprin AV (75/20)
On regular at home monitoring of blood glucose levels which were within the normal range, he stopped taking Tab Metformin.
On 14th March 2020 he paid a visit to our hospital with the similar complains and a review scan of 2DEcho was done which revealed end point septal separation distance to be increased and Tab Vymada was increased to 100mg.
On July 28th, 2020 he presented to our OPD with the complains of Dyspnea at rest since 5 days which apparently aggravates when the patient is in supine posture and he also complains of occasional cough with scanty mucoid, non blood tinged sputum especially while he is asleep. He says he developed bilateral pedal edema extending upto his knee over the past 4 days followed by abdominal distension.
Patient appears to have gained weight with abdominal girth measuring 116cm and he weighed 101 kg
He weighs 93 kgs now
He appeared to be in respiratory distress with a respiratory rate of 28 cycles per minute and his saturation was at 98 % on room air.
His heart was beating at 120 bpm with a blood pressure of 100/70mmhg.
He was afebrile.
He had Icterus
His JVP was raised
CVS:
On palpation: His apex beat was in 6th intercostal space, 1cm lateral to midclavicular line.
On auscultation, S1 S2 +
His lungs were clear on auscultation
His abdomen was soft to palpate and bowel sounds were heard.
CNS: Normal
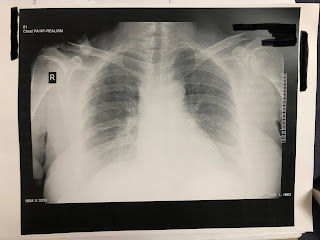
ECG & CHEST X RAY PA VIEW:
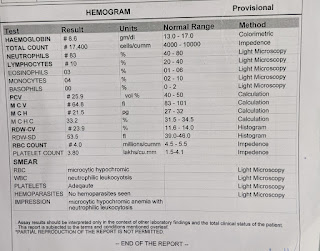
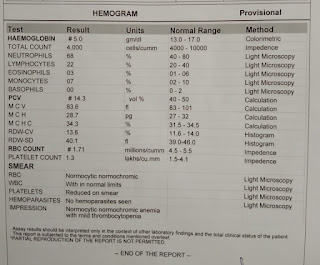
HEMOGRAM:
Hb - 13g/dl
TLC - 7000 cells/cumm
Platelet count - 2.28 L/cumm
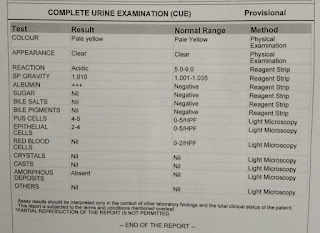
Complete Urine Examination:
showed no albumin, sugars, RBCs
2-4 Pus & epithelial cells
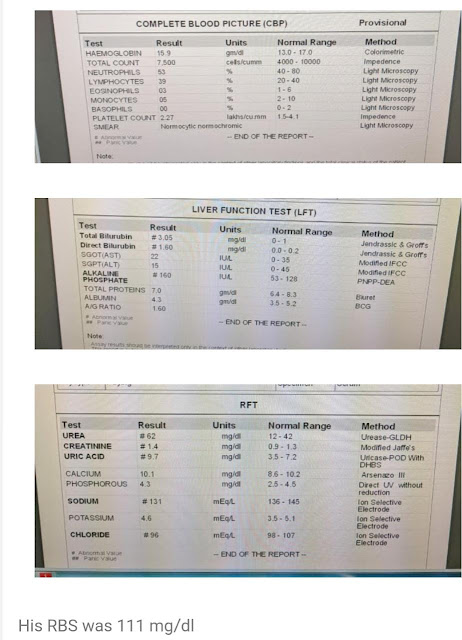
Renal Function Test:
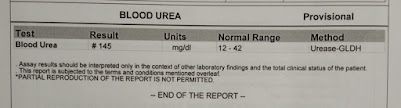
Urea - 53 mg/dl
Creatinine - 1.4 mg/dl
Uric Acid - 9 mg/dl
Calcium - 9.6 mg/dl
Phosphorus - 3.3 mg/dl
Sodium - 133 mEq/L
Potassium - 4 mEq/L
Chloride - 98 mEq/L
Liver Function Test:
Total Bilirubin - 4.60 mg/dl
Direct Bilirubin - 2.42 mg/dl
AST - 56 IU/L
ALT - 44 IU/L
ALP - 129 IU/L
Total Proteins - 6.2 gm/dl
Albumin - 3.9 gm/dl
His 2Decho showed dilated chambers with global hypokinesia, ejection fraction of 26 %, severe MR, mild TR, Trivial AR, mild pericardial effusion, mild PAH and IVC measuring 1.7 cms.
The Patient is currently on fluid and salt restriction Along with INJ LASIX 40MG TID
TAB VYMADA 100 MG BD
TAB VALSARTAN 80MG OD
TAB MET XL 12.5MG OD
TAB DYTOR PLUS 10/25 OD
THESIS
August 09, 2021
TITLE;
"LIVER FUNCTION TESTS IN TYPE II DIABETES MELLITUS IN RURAL TERITIARY CARE CENTRE”
INTRODUCTION:
Diabetes mellitus is a complex metabolic condition defined by level of hyperglycemia giving rise to micro vascular and macro vascular complications 1 .
Current estimates suggests that there are 170 million people suffering from DM worldwide and this number is going up to 266 million by 20302.The prevalence of DM in India is around 31 million and this number will increase to 80 million by 20302.
Indians develop diabetes at younger age, with lower degree of obesity and have increased risk of chronic diabetic complications. Hence DM is a major public concern in India. Various complications related to micro or macro vascular diseases like retinopathy, nephropathy, neuropathy, ischemic heart diseases and peripheral vascular disease have been reported. Liver diseases are often overlooked as a complication of DM.
Infact VERONA-DIABETES POPULATION BASED STUDY has shown that among patients with DM standardised mortality rate from cirrhosis was higher than cardiovascular diseases 3.Though association of diabetes with cirrhosis has been recognised for more than 100 years, liver diseases in diabetes remains under estimated 4.
Abnormal liver function test results are more common in diabetes mellitus than in the non-diabetic population as well as in patients with type 2 diabetes than in those with type 1 diabetes. Elevated activities of the two serum transaminases; alanine transaminase (ALT) and aspartate transaminase (AST) may be associated with liver disease. Elevation of these enzymes is strongly related to obesity, diabetes and dyslipidemia, and their measurement may act as a surrogate marker of NAFLD presence.
This study was conducted to estimate the prevalence of elevated liver transaminase levels among patients with type 2 diabetes and to determine the associated risk factors.
AIM:
To assess the pattern of liver function test in type 2 diabetes milletus.
OBJECTIVES:
To determine the liver function tests (serum bilirubin, AST, ALT, alkaline phosphatase) in patients with type II diabetes mellitus.
To determine the associated risk factors for abnormal liver function tests in patients with type II diabetes mellitus.
PATIENTS AND METHODS:
PLACE OF STUDY: Department of General medicine Kamineni Institute of Medical Sciences, Narketpally
STUDY PERIOD: October 2018-September 2020
STUDY DESIGN: Cross-sectional study
SAMPLE SIZE: 80
INCLUSION CRITERIA:
• Presence of type 2 diabetes Mellitus in patients above the age of 40 years
• Duration of type 2 diabetes Mellitus at least 1 year and above.
EXCLUSION CRITERIA:
1. Age less than 40 years.
2. Duration less than one year.
3. Consumption of alcohol.
4. Seropositivity of HbsAg and antiHCV antibody.
5. Seropositivity of HIV ELISA.
6. Patient on drugs proven to cause steatohepatitis (steroids, amiodarone, oral contraceptive pills, and other estrogen containing preparations).
7. Patients with renal failure and cardiac failure.
METHODOLOGY:
The study was approved by the ethics committee of Kamineni Institute of Medical Sciences, Narketpally.
All patients satisfying the inclusion criteria are enrolled in the study.
A written informed consent has been taken from the patients prior to the start of the study.
Measurement of height, weight, waist circumference, hip circumference and calculation of BMI and waist to hip ratio.
A total of 80 type 2 diabetic patients who met the inclusion criteria were studied during this period. Both inpatients and outpatients attending outpatient department were included in the study.
Body weight was taken while the patients barefooted and in light clothing, using a weighing scale with accuracy of ±100 g. Standing height was measured without shoes to the nearest cm with the shoulders in a relaxed position and the arms hanging freely. Body mass index. (BMI) (kg/m 2) was calculated as the ratio of weight (kilograms) to the square of height (meters). Patients' BMI was classified according to WHO classification, as being normal (BMI; 18.5 to 24.9 kg/m 2), overweight (BMI; 25 to 29.9 kg/m 2) or obese (BMI>30 kg/m 2).
Waist circumference and hip circumference was measured in a standing position using non stretchable tailor measuring tape to look for central obesity. Central obesity is defined in men by a waist-to-hip circumference ratio greater than 1.0 or a waist circumference greater than 40 inches (102 centimetres). In women, central obesity is defined by a waist-to-hip ratio greater than 0.8 or a waist circumference greater than 35 inches (88 centimetres).
All the above patients were examined and screened for HbsAg, anti-HCV antibody, HIV ELISA and were found to be negative. Morning samples of venous blood were collected from patients after fasting for at least 14 hours and tested for glucose, urea, Creatinine (using semi auto analyser Merck 300), haemoglobin A1C 35 (HbA1C) [Using High Performance Liquid Chromatography method], for the liver enzymes; ALT and AST [Using semi auto analyser Merck 300], and for lipid profile including total cholesterol (TC), high density lipoprotein (HDL), triglycerides (TGL), and low density lipoprotein (LDL)[ Using semi auto analyser Merck 300] and serum protein, albumin, globulin(Using calorimetry photochem -5). Elevated ALT and AST levels were defined as enzyme activity >40 U/L respectively, according to the clinical assay adopted by the centre‘s laboratory.
Ultrasound abdomen was done for all patients, to look for size of the liver, echogenicity of liver parenchyma, any evidence of chronic liver disease like coarse echo texture of liver, dilated portal vein and/or splenomegaly. The diagnosis of fatty liver was based on a diffuse hyperechoic echo texture (bright liver) and increased liver echo texture compared with the kidneys.
INVESTIGATIONS:
Complete blood picture
Complete urine examination
HbsAg
AntiHCV antibody
HIV ELISA
Blood sugar: FBS, PLBS
HbA1C
Blood urea
Serum Creatinine
Serum electrolytes
Liver function test
Serum bilirubin
Direct bilirubin
Indirect bilirubin
Aspartate transaminase
Alanine transaminase
Alkaline phosphatase
Serum total proteins
Albumin
Fasting Lipid Profile
Total cholesterol
HDL
LDL
VLDL
Triglycerides
Ultrasound abdomen
ECG
LINK TO COMPLETE THESIS WITH MASTER CHART
A 44 year old man presented with a 3-day history of bilaterally symmetrical rapidly progressive generalized edema.
Present Illness
An agile stonemason, the patient reported that this symptom first started suddenly 3 days ago, at night, when he noticed he started feeling facial puffiness with pedal edema. The next morning, while brushing his teeth, the patient noticed he had facial puffiness, in the mirror. At the same time, he also noticed that he developed bilaterally symmetric, pitting type pedal edema, extending upto the middle of his legs. He immediately presented to the hospital with these complaints.
On interviewing the patient further, he denied having breathlessness, palpitations or chest pain. He reported frothing of urine but no haematuria. He also reported gradually decreasing urine output over the past 3 days. He did not have pain during micturition, no pus or any other abnormal discharge (casts) in urine. He did not have any history of vomiting or diarrhea, no history of acute retention of urine, no prior history of fever or rash, no history of antibiotic usage or any drugs in the past 1 week. The patient also denied any history of yellowish discoloration of skin or sclera.
Prior to this, the patient reported that since 2011, he had severe joint pains, which were initially asymmetric and gradually became bilaterally symmetrical and involving the small joints of his hands and wrist. The joint pains were associated with significant local edema, and painful limitation of movements, which made his job (stonemasonry) difficult.
[Other activities which were painful and difficult for the patient were -
Holding his cup of tea or glass of water,
Pain in his finger joints and wrist while brushing,
Pain while holding mug when taking bath and
Pain in toes and ankles on both sides when walking)]
He reported that he also had debilitating early morning pains and limitation of movements in his hands, wrists and feet, which usually lasts for about an hour, He reported that the pains and limitation of movements improved with activity, with gradual reduction in edema of joints.
From 2011 to 2019, these joint symptoms gradually progressed in severity, now also involving several large joints (shoulders, elbows, knees and hips) warranting several medical consults, where he was frequently prescribed pain killers. The patient did not have any documentation of the pain killers he took in these 8 years. In December 2020, he presented to our hospital with similar complaints of joint pains, when he was prescribed with Etoricoxib and Febuxostat (he had hyperuricemia). He reported that his symptoms alleviated with these drugs but he intermittently had worsening of same symptoms in the interim. The patient denied any history of skin rash, photosensitivity, nasal or oral ulcers, chest pain or abdominal pain, weakness in his limbs (such as difficulty in taking stairs or lifting heavy stones and nor any weakness in his distal aspects of limbs such as mixing food, buttoning his shirt or holding a glass or slipping of footwear), isolated single joint pain or edema, or a past history of kidney stones. He also does not have any history of difficulty in swallowing, altered bowel habits, pain in the pulp of his digits, or painful tearing, photophobia or visual loss. He also denied any history of gritty sensation in eyes or dryness of mouth.
Apart from these, the patient reported that, for the past 3 days, he has burning sensation in his eyes with increased tearing but no visual deficits. He also reported for the past 1 year, he developed subcutaneous swellings in the proximal joints of his fingers. He denies any history of early satiety or post prandial fullness or pain. He reported that his clothes have slightly loosened over the past 1 year with involuntary weight loss and loss of appetite. He denies having a history of wrist or foot drop, chest pain, palpitations or breathlessness. No history of loss of consciousness, falls or tingling or numbness in his feet or hands.
Past History
No significant past history.
Medical/Surgical History
Chronic intermittent use of analgesics (type and dose unknown). Has been using Etoricoxib 60 mg and Febuxostat 80 mg intermittently for the past 8 months. No relevant surgical history. No history of allergy or atopy.
Personal History
The patient had been working as a stonemason for the past 20 years. He is a devout Catholic Christian and a strict teetotal (has never smoked or consumed alcohol in his life). He stays with his wife and 2 children (elder son and younger daughter) in Miriyalguda. He is from a close-knit family and regularly socialises with his family (parents and his 2 elder brothers). Apart from his troubling joint pains, he used to a have a fairly balanced and good quality of life, with good sleep every night, good appetite and adequate access to nutritious food and clean drinking water. He also had a balanced social well-being with a tightly-knit community at home and his church.
However, since the last 1 year, his appetite started to decrease and he also involuntarily lost weight. His bowel and bladder habits have always been normal but these joints pains have forced him into early voluntary retirement from his job in 2019. His and his family's finances have been supported by his brothers and from generous donations from his church. He feels his mental health has remained intact, thanks to his supportive family and fellow churchgoers.
Family History
No significant family history reported.
Social & Educational History
Married for 18 years with 2 children. Primary education upto Class 7 in Telugu medium.
Immunization History
None taken since birth.
Problem Representation / History Analysis
A 44 year old stonemason from Miriyalguda, presented with a 3 day history of anasarca, frothy urine and gradually decreasing urine output, on a background of a 10 year history of chronic bilaterally symmetric polyarthritis (evidenced by severe pain, edema and limitation of joint movements).
Localisation of Acute Problem
Anasarca and frothy urine with decreasing urine output suggest a renal pathology. Proteinuria causing anasarca likely due to glomerular pathology. Other systemic causes like heart failure and liver dysfunction can be ruled out due to absence of dyspnea, palpitations, bendopnea or syncope. Liver dysfunction can be ruled out by lack of jaundice, melaena or hematemesis (from bleeding varices), and abdominal distention not occurring prior to pedal edema
Within the kidney, pre-renal and post-renal causes can be effectively ruled out from the absence of volume loss (vomiting, diarrhea, diuretic abuse or burns) and no history of acute retention of urine or lower urinary tract symptoms (LUTS) like frequency, urgency, hesitancy or precipitancy. The presence of frothy urine and edema strongly supports a glomerular pathology due to significant loss of protein and also decreased urine output. Isolated defects in tubular/interstitium are unlikely as such patients have a deficit in maintaining urinary concentration, which causes polyuria. Such a high range of proteinuria causing anasarca is also not seen with tubular/interstitial pathologies alone.
Provisional Diagnosis - Acute Glomerulopathy (Glomerulonephritis / Nephrotic syndrome)
Features to look for -
1. Hypertension (secondary hypertension in Glomerulonephritis)
2. Haematuria on Urine Microscopy (particularly dysmorphic RBCs in urine)
3. Quantification of Proteinuria
4. Serum Albumin / Total Proteins
5. Urine specific gravity / calculated urine osmolality to check for isosthenuria (to look for secondary tubular/interstitial damage)
6. Renal biopsy, if diagnosis remains uncertain
Localisation of Chronic Problem
This 44 year old man has a 10 year history of bilaterally symmetrical progressive inflammatory polyarthritis. Features favouring an inflammatory pathology are -
1. Features of inflammation such as severe pain associated with edema of the joints and limitation of range of active movements
2. Early morning stiffness, lasting for more than 30 mins (for 1 hour in this patient)
3.Pain and edema of joints improving with activity and worsening with rest
4. Features of uncontrolled systemic inflammation such as fever, involuntary loss of weight associated with loss of appetite.
5. Swellings at joints and deformation of normal joint posture
Provisional Diagnosis - Bilaterally Symmetric Chronic Progressive Inflammatory Peripheral Polyarthritis
Clinical Examination
Initial examination revealed, the patient was conscious, coherent and co-operative, lying in bed in supine position. He was in some visibly apparent distress with flexion at his elbows and wrists, bilaterally, which were mildly painful when resting on the bed and his abdomen, respectively. The patient was dressed in a round neck t-shirt and when asked to sit up and take his t-shirt off, he had significant pain and limitation of movements at multiple joints but no weakness.
Vitals were taken in supine and sitting position -
Supine Position
Pulse - 92 bpm, regular, normal volume, condition of vessel wall - normal, no radio-radial or radio-femoral delay. All peripheral pulses were normal.
Blood Pressure - 140/90 mmHg
Temperature - 99.3F
Respiratory Rate - 24 cycles per minute. Mildly acidotic + (with prolonged duration of expiration)
Sitting Position
Pulse - 96 bpm, regular, normal volume, condition of vessel wall - normal, no radio-radial or radio-femoral delay.
Blood Pressure - 150/90 mmHg
Head to Toe General Examination
General Condition - Fair built and appears well nourished.
Hair - Thin and slightly greyed. Not easily pluckable or no areas of scarring or non-scarring hair loss. No lesions noted on the scalp.
Eyes - No conjunctival chemosis or injection, No redness or corneal lesions. Bilateral, purplish reticular markings noted on the sclera of both eyes. Palpebral conjunctival pallor +. No icterus. No cyanosis. Bilateral Periorbital puffiness +
| Periorbital Edema +. Pallor was also + |
General Head, Neck & ENT - No abnormalities. No lymph node enlargement.
Axial - No apparent spinal deformities
Fingers and Nails - Leukonychia +. No clubbing or cyanosis. Capillary refill time - 2 seconds.
Bilateral pitting type pedal edema +, extending upto middle of legs.
Systemic Examination
Musculo-Skeletal System
Inspection - No visibly apparent spinal deformities;
Palpation - Inspectory findings confirmed. No spine tenderness.
Movements - Atlanto-occipital - Flexion, extension and lateral flexion normal
Atlanto-axial - Rotation of head normal
Spinal Flexion, Spinal Extension, Lateral Flexion and Rotation are normal
Appendicular Skeleton - Upper Limbs (Positive Findings)
Shoulders (both sides) -
- Inspection - Attitude - Slightly flexed and internally rotated; Contour normal; No edema or erythema
- Palpation - Mild increase in temperature on both sides
- Range of Movements - Mild Active and Passive limitation of all range of movements (flexion, extension, adduction, abduction, internal rotation and external rotation)
Elbows (both sides) -
- Inspection - Attitude - mid-flexion; alignment of elbow and forearm - normal; Edema +; No scars or sinuses; no muscle wasting
- Palpation - All Inspectory findings are confirmed; Raised temperature +; Edema +; Wincing on touch +; Fluctuation test +; 3-point bony relationship intact
- Range of Movements - Severe pain on active movements of flexion, extension; Mild pain with supination and pronation;
Wrists (both sides) -
- Inspection - Attitude - Mild extension; Radial deviation of wrists +; Diffuse edema +; Redness +;
- Palpation - All Inspectory findings confirmed; Temperature raise +; Wincing on touch +;
- Range of Movements - Severely limited and extremely painful active movements of flexion, extension, radial deviation and ulnar deviation.
Hands (both sides) -
- Inspection - Attitude - Palmar subluxation and Ulnar deviation of the MCP joints; Swollen and Erythematous PIP joints; No swelling or redness of DIP joints; No apparent muscle wasting; Mild hyper-extension of PIP of thumbs; Pulp of fingers normal
- Palpation - All Inspectory findings are confirmed; Temperature raise +; Wincing on gentle palpation of MCP joints and PIP joints; Palpation of DIP joints is normal; Swellings also + on 3rd and 4th PIP joints on both sides. Z-deformity +.
- Range of Movements - Severe pain and severe limitation of active movements of flexion, extension and ulnar and radial deviation of MCP joints; severe pain and limitation of active and passive movements of flexion and extension at PIP joints. DIP joints normal.
Appendicular Skeleton - Lower Limbs (Positive Findings only)
Hip Joints (both sides)
- Limitation of passive movements of flexion and extension (towards the end of range of motion);
Knee Joints (both sides)
- Inspection - Swelling and erythema +; Attitude - flexion;
- Palpation - All Inspectory findings are confirmed; Raised temperature + ;
- Range of movements - Severe pain and limitation of active and passive movements of flexion and extension and lateral and medial rotation; (Patient was unable to stand on Day 1 and was able to stand on Day 2 with analgesic use).
Ankles (both sides)
- Mild pain and limitation of active and passive movements of plantar flexion and dorsiflexion; Mild pain and limitation of movements of inversion and eversion.
- Palpation of Achilles tendon is normal.
Foot examination (both sides)
- Mild pain and limitation of passive movements of flexion and extension of MTP joints; great toe flexion and extension normal;
Other Systems Examination
Cardiovascular System - No abnormalities detected
Respiratory System - No abnormalities detected
Abdominal Exam - No abnormalities detected
Nervous System - No deficits detected
Investigations
 |
| X-ray AP view of the hands and wrists - Osteopenia and erosions of the MCP and PIP joints are noted. Scallop sign +. Significant soft tissue swelling is also noted. |
With a provisional diagnosis of Acute Glomerulopathy on the background of bilaterally symmetric chronic progressive erosive peripheral polyarthritis, features supporting the diagnosis of glomerulonephritis were -
- Secondary Hypertension
- Oliguria (360 ml urine in the last 24 hours)
- Hypoalbuminemia (Serum Albumin 2.5g/dl) and Anasarca
- Dysmorphic RBCs in Urine
(A review of literature was done to evaluate the sensitivity and specificity of dysmorphic RBCs for glomerular disease pathologies - One study conducted in Bangladesh showed that urinary dysmorphic RBCs were 92.7% sensitive and 100% specific for a biopsy confirmed diagnosis of glomerulonephritis. [1]
Similar values of sensitivity and specificity was also confirmed in another study jointly conducted in Australia and China, where glomerulonephritis was confirmed with renal biopsy. [2])
Thus, with glomerular disease being most likely, an anatomical diagnosis is made. The etiological cause for glomerular injury needs to be ascertained.
A careful construction of the problem representation for this patient and insight into the sequence of his life events can provide clues that the current acute problem could be a sequelae of his long term, poorly treated chronic problem.
Thus, a good clinical diagnosis of his musculo-skeletal problems is required to get a better picture of his current illness.
The patient has Bilaterally Symmetrical Chronic Progressive Erosive Peripheral Polyarthritis. Differential diagnosis for such conditions include -
1. Rheumatoid Arthritis (most likely)
2. Rheumatoid Arthritis with coexistent Gout
3. Psoriatic Arthritis
4. Enteropathic Arthritis
5. Reactive Arthritis
6. SLE
7. Polymyositis / MCTD (Mixed Connective Tissue Disorder) (least likely)
With Rheumatoid Arthritis being most likely, ACR/EULAR classification criteria can be applied for diagnosis -

|
This patient has >10 joints involved with multiple small joints involvement - 5 points; Symptom duration 10 years - 1 point; RA Factor - NEGATIVE; CRP elevated & ESR - 120 mm/hr - 1 point; Total Score - 7/10 [3]
Thus, a diagnosis of Rheumatoid Arthritis is likely. The clinical utility of RA factor came into question. A review of literature showed that sensitivity of RA factor for Rheumatoid Arthritis was 28% and specificity was 87%. For non RA rheumatological disorders, the sensitivity was 29% and the specificity was 88% [4]. Thus, the authors concluded that (due to high specificity and NPV), the test is best ordered when the suspicion for a rheumatological is low but just high enough, that a negative result would increase the post-test probability of a rheumatological disorder being unlikely.
This patient had a chronic history of symmetric small joint and then large joint inflammatory peripheral polyarthritis, With minor erosions notable in the PIP and MCP joints of both hands, classification criteria are diagnostic for Rheumatoid Arthritis.
No history of skin rash (psoriatic arthritis) or chronically altered bowl habits (enteropathic arthritis); No history of dysuria or burning pain during micturition or a history of severe burning pain in eyes with photophobia and excessive tearing or discharge (reactive arthritis) makes the other diagnoses unlikely.
Epidemiologically, SLE occurs more commonly in females at a ratio of 9:1, coupled with this, the absence of other features of SLE, such as alopecia, photosensitivity rash, nasal or oral ulcers, serositis, hemolytic anemia etc. makes this diagnosis very unlikely.
The absence of muscle weakness, muscle pain and the presence of destructive arthritis makes Polymyositis / MCTD extremely unlikely (Polymyositis usually causes nonerosive arthritis).
Thus the current acute glomerulonephritis can be framed in the background of Chronic Poorly Treated Rheumatoid Arthritis.
4 scenarios are possible -
1. Poorly treated RA causing Secondary Amyloidosis (most likely) Secondary amyloidosis is most commonly seen in chronic poorly treated systemic inflammatory syndromes. This study shows that secondary amyloidosis is the most common cause of rapidly progressive glomerulonephritis in patients who were untreated for more than 10 years. [4] Coupled with features of amyloidosis of the heart, this is the most likely cause of his renal dysfunction.
2. Vasculitic Glomerulonephritis (IgA Mediated)
The incidence of IgA nephropathy in patients with RA is similar to that in the general population. [5]
3. Primary Glomerulonephritis (Idiopathic)
These include Mesangial / Mesangio-proliferative glomerulonephritis; Membranous Nephropathy; FSGS [6]
4. Renal Dysfunction secondary to drug use (less likely)
Most commonly implicated drugs causing nephritic/nephrotic syndrome are Gold and Pencillamine, neither of which the patient used. The patient had chronic intermittent use of Etoricoxib but NSAIDS usually cause Tubulo-interstitial nephritis and not nephrotic syndrome.
5. Crystal Nephropathy (less likely) Gout crystals precipitate at a pH of 7.0 and often precipitated in the collecting ducts in the medulla, causing Acute Tubular Necrosis with little interstitial or glomerular involvement.
Final Diagnosis - A 44 year old, who presented with a 3 day history of anasarca and decreased urine output is diagnosed with -Acute Glomerulonephritis, likely due to Secondary Amyloidosis due to Chronic Poorly Treated Seronegative Erosive Rheumatoid Arthritis.
Dilutional Hyponatremia secondary to Anasarca due to Glomerulonephritis
Hyperuricemia likely due to decreased Uric Acid Excretion Precipitating Gouty Arthritis
Anemia of Chronic Disease secondary to Poorly Treated Rheumatoid Arthritis.
Further PlanAbdominal Fat Pad Biopsy for Amyloidosis Needle Aspiration of Synovial Fluid for Crystal Induced Arthritis (Gout) Treatment- Free water restriction for Hyponatremia
- Tab. PREDNISOLONE P/O 20 mg OD
- Tab FEBUXOSTAT P/O 80 mg OD
- Haemodialysis for worsening renal dysfunction
Pedagogic Questions- Abdominal fat pad biopsy vs Renal biopsy ?
The clinical data and biopsy results of 194 SA patients who were treated in Peking Union Medical College Hospital from January 2009 to June 2015 were retrospectively analyzed. Results The highest sensitivity was achieved by biopsy of affected organs, with renal biopsy 97.4%, heart biopsy 95.0% and liver biopsy 87.5%. Among non-invasive biopsy methods, tongue biopsy was found to be 75% sensitive, followed by gingiva biopsy at 57%, abdominal fat pad aspiration at 57%, rectum biopsy at 16%, and bone marrow examination at 8%. Combination of tongue and abdominal fat pad biopsy yielded a detection rate of 93.1%. Conclusions Biopsy of the involved organ has the highest sensitivity. However, combination of multiple non-invasive biopsy methods may has sensitivity comparable to organ biopsy and is safer and more convenient. [7] 2. Single DMARD vs Combination therapy ? A Cochrane review, published in The BMJ [8] looked at the clinical efficacy of Methotrexate monotherapy vs Combination therapy (MTX + Non-biological or MTX + Biologicals). Data of Methotrexate -naïve patients was gleaned from this meta-analysis - Outcomes - The major outcomes of the review were American College of Rheumatology (ACR) 50 response, a composite measure of improvement in disease activity (dichotomous outcome); radiographic progression, measured by Larsen, Sharp, or modified Larsen/Sharp scores (continuous outcome); and withdrawals due to adverse events, including death (dichotomous outcome). 3. When to initiate dialysis? How long can we wait? Ex tempore interpretation of the AKIKI-2 trial. [9] 4. Can Rheumatoid Arthritis and Gout co-exist together? The study population included 813 patients, 537 (66%) were rheumatoid factor positive; 33% had rheumatoid nodules, and 53% had erosive joint disease. During 9771 total person-years of follow-up (mean 12.0 years per RA patient), 22 patients developed gout by clinical criteria. The great toe was the most common site of gout (12 of 22 patients). The 25 year cumulative incidence of gout diagnosed by clinical criteria was 5.3%. Typical intracellular monosodium urate crystals were present in 9 of 22 patients with acute gout; all had developed gout after the RA incidence date. The 25 year cumulative incidence of gout diagnosed by clinical criteria including presence of urate crystals is 1.3%. The prevalence of gout in RA on Jan 1, 2008 was 1.9% (11 of 582 patients) as opposed to expected prevalence of 5.2% (or 30 patients) based on National Health and Nutrition Examination Survey (NHANES) data using age and sex specific prevalence rates. [10] 5. Efficacy of Febuxostat vs Allopurinol for Gout ?
[11]
|
References- Sultana T, Sultana T, Rahman MQ, Rahman F, Islam MS, Ahmed AN. Value of dysmorphic red cells and G1 cells by phase contrast microscopy in the diagnosis of glomerular diseases. Mymensingh Med J. 2011 Jan;20(1):71-7. PMID: 21240166.
- Pollock C, Liu PL, Györy AZ, Grigg R, Gallery ED, Caterson R, Ibels L, Mahony J, Waugh D. Dysmorphism of urinary red blood cells--value in diagnosis. Kidney Int. 1989 Dec;36(6):1045-9. doi: 10.1038/ki.1989.299. PMID: 2689749.
- https://www.eular.org/myUploadData/files/RA%20Class%20Slides%20ACR_Web.pdf.
- Helin H, Korpela M, Mustonen J, et al. Renal biopsy findings and clinicopathologic correlations in rheumatoid arthritis. Arthritis Rheum 1995;38(2):242–7.
- Korpela M, Mustonen J, Helin H, et al. Immunological comparison of patients with rheumatoid arthritis with and without nephropathy. Ann Rheum Dis 1990;49(4): 214–8.
- Horak P, Smrzova A, Krejci K, et al. Renal manifestations of rheumatic diseases. A review. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2013;157(2):98–104.
- Zhang CL, Feng J, Cao XX, Zhang CL, Shen KN, Huang XF, Zhang L, Zhou DB, Li J. Selection of Biopsy Site for Patients with Systematic Amyloidosis. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2016 Dec 20;38(6):706-709. doi: 10.3881/j.issn.1000-503X.2016.06.013. PMID: 28065238.
- Hazlewood GS, Barnabe C, Tomlinson G, Marshall D, Devoe DJ, Bombardier C. Methotrexate monotherapy and methotrexate combination therapy with traditional and biologic disease modifying anti‐rheumatic drugs for rheumatoid arthritis: A network meta‐analysis. Cochrane Database of Systematic Reviews. 2016(8).
- Gaudry S, Hajage D, Martin-Lefevre L, Louis G, Moschietto S, Titeca-Beauport D, La Combe B, Pons B, De Prost N, Besset S, Combes A. The Artificial Kidney Initiation in Kidney Injury 2 (AKIKI2): study protocol for a randomized controlled trial. Trials. 2019 Dec;20(1):1-0.
- Jebakumar A, Crowson C, Udayakumar D, Matteson E. Co-Existence of Gout in Rheumatoid Arthritis: It Does Happen! A Population Based Study.: 134. Arthritis & Rheumatism. 2012 Oct;64.
- Huang X, Du H, Gu J, Zhao D, Jiang L, Li X, Zuo X, Liu Y, Li Z, Li X, Zhu P. An allopurinol‐controlled, multicenter, randomized, double‐blind, parallel between‐group, comparative study of febuxostat in C hinese patients with gout and hyperuricemia. International journal of rheumatic diseases. 2014 Jul;17(6):679-86.
SHORT CASE-1:
CASE PRESENTATION
History taken from Patient and Attendant (elder brother); Reliability 9/10.
A 49 year old English and Telugu language lecturer presented with a 2 month history of progressive asymmetric involuntary movements of his right index and middle fingers
Present Illness
The patient reports that he first noticed them happening nearly 6 months ago, which was very small in amplitude, affecting these two fingers only. He says that these movements often worsened with rest and abated with activity. They were not troublesome initially but for the past 2 months he has been unable to correct answer sheets because of the involvement of his thumb and maintaining stability of his hand was proving difficult. He describes these movements as involuntary, rhythmic to and from oscillations.
He also adds that his handwriting has become ugly with very small letters. On interviewing further, the patient reports that he feels stiffness in his wrists (Right>Left), which has now ascended to his elbows. He says the stiffness is present throughout the range of motion. He also says that since the last 1 month, the same involuntary movements also started appearing in his left hand.
At this point, he also says that his walking has become difficult with small, short steps and a forward stoop, and he feels that although he weighs 60 kgs. he feels like it weighs 100 kgs.
He does not report any difficulty in reading the newspaper, holding the paper, turning pages or folding it back. He does not have any difficulty in brushing his teeth or combing his hair. He also denies having difficulty in holding objects, such as holding a water bottle to drink nor any difficulty in mixing food and eating it. He does not have any difficulty in wearing a vest or in buttoning or unbuttoning his shirt. No difficulty in lifting his lower limbs and wearing a trouser.
The interview continues and we question for any difficulty in taking the stairs - he reports that he has been having difficulty in taking stairs up, in that he feels he sometimes might lose balance. He has no difficulty in descending stairs. The patient also denies having swaying of his trunk while walking or overshooting his hand while picking up objects.
On pressing further - he reports that he hasn't been having morning erections since 2 months and also reports a loss of sexual desire. He also says that since 2 months his bowel habits have been incredibly erratic, in that he sometimes has an immediate urge to defecate when he has tea and sometimes goes 2 to 3 days with constipation.
He, however, denies feeling dizzy or lightheaded when waking up in the morning. He denies having stiffness in his lower limbs, denies cotton wool sensation of floor, denies burning pain or inability to feel hot or cold stimuli. He also denies buckling of knees but, however, he reports that he has been having a great difficulty to walk in the dark since 2 months and says that he feels like he would definitely fall without support.
His brother gives a positive affirmation for all his symptoms and also says that he previously used to be a fairly jovial and hardworking man with good oratory skills, however, since the last 2 months he says his brother's speech lacks that 'edge' which he previously had. On asking further, the brother says that he has been speaking in a monotonous drab since 2 months.
The patient and his brother deny noting any fluctuations in his alertness, apathy or emotional instability to family or personal issues, no history of visual hallucinations, no history of incoherence of speech or irrelevant talk and no history of difficulty in managing finances or poor self care.
The patient denies ever having urinary incontinence, memory deficits, the brother vehemently denies the patient ever being anti-social, he does not have any difficulty in forming new memories or any visual deficits.
Past History
No similar complaints in the past. No history of Diabetes, Hypertension, Coronary Artery Disease, Seizures, Asthma or Tuberculosis.
Medical/Surgical History
The patient is not on any medications. He also did not report usage of any herbal or alternative medicine. He has no past surgical history.
Personal History
The patient is a teacher; he teaches English and Telugu for B.com and B.sc students in a college in Miriyalguda. He has been in this profession for the last 9 years. He has a triple M.A. in English, Sanskrit and Telugu.
The patient neither smokes nor drinks, he had a fairly routine lifestyle with waking up early in the morning and getting ready for his job. However since the lockdown, he had to stay at home with his college shut. He spends most of his time reading the newspaper and other literature. He lives with his wife and one son, who is studying Inter 2nd year. His sleep habits are well maintained. However, his bowel habits have changed in the last 2 months as detailed above. His appetite is good, he consumes vegetarian food on most days with a good access to nutritious food and clean drinking water. He occasionally enjoys non vegetarian food. He socialises well with his extended family and his local community. He is well respected among his peers and students alike.
Family History
No significant family history reported.
Social & Educational History
Married for 24 years with 1 child. Triple degree in MA in English, Sanskrit and Telugu.
Immunization History
Complete upto age 5.
General Examination
Patient is conscious, coherent & cooperative.
Vitals at the time of history taking -
PR - 88 bpm
BP - 190/110 mm Hg
After standing for 3 mins - BP - 160/110 mm Hg
Temp - Afebrile
RR - 16 cpm
No signs of Pallor, Icterus, Cyanosis, Clubbing, Generalized lymphadenopathy or edema.
Nervous System Examination.
Higher Mental Functions
1. Level of consciousness - Normal (CGS15/15)
2. Attention - Intact.
3. Orientation - to time, place and person - Intact
4. Language - fluency & latency, comprehension, repetition, naming, reading and writing - Intact. Prosody - impaired
5. Memory - immediate recall, recent and remote - Intact
6. Other higher mental functions - general knowledge, abstraction, judgement, insight and reasoning - Intact.
MMSE
29/30 (No cognitive impairment)
CN Examination
1st
Normal (smell of soap).
2nd
Counting fingers at 6mts both eyes normal.
3rd,4th,6th
Pupil size. N N
DLR/CLR. N. N
No pstosis, nystagmus.
5th
Both sensory & motor normal.
Corneal & Conjunctival reflex +.
7th
Nasolabial fold normal.
No deviation of mouth.
Salivation & Lacrimation unaffected.
8th
Rinne's AC>BC.
Weber's - No lateralization.
9 th, 10th &
Palatal movements normal.
No difficulty in swallowing.
Gag reflex present.
11th
Movements of neck in all directions+.
Lifting of shoulders +.
12th
Tone of tongue - Normal.
No wasting, no fibrillations & deviation of tongue.
Tongue tremor+.
MOTOR SYSTEM
Right. Left
✓Bulk Normal Normal
✓Tone
Upper limb R. L
Shoulder Normal Normal
Elbow Normal Normal
Wrist Hypertonia Normal
(Cog wheel rigidity)
Lower limb Normal Normal
✓Power
UL
Proximal 5/5 5/5
Distal 5/5 5/5
LL
Proximal 4/5 4/5
Distal 5/5 5/5
✓Reflexes
Superficial reflexes
Right Left
Corneal + +
Conjunctival + -
Abdominal + -
Plantar - -
Deep tendon reflexes
Right Left
Biceps 2+ 2+
Triceps 2+ 1+
Supinator 1+ Absent
Knee 3+ 3+
Ankle 1+ 1+
Clonus Absent. Absent
Involuntary movements - Resting tremors of Right upper limb 3-4Hz, high amplitude.
Gait - Reduced arm swing.
Finger tap and toe tap - Normal.
No decrease in speed on repeating the movement continuously.
✓SENSORY SYSTEM
Right Left
Pain + +
Fine touch + +
Temperature + +
Vibration
Medial malleolus 5.7s 4.6s
Patella 9s 4.3s
Elbow 4.8s 6.4s
Wrist 5s 7s
Proprioception Normal Normal
Stereognosis Normal
✓CEREBELLUM
Titubation - absent
HINTS
Head Impulse - negative
Nystagmus - negative
Test for skew - negative
Gait Ataxia absent.
Dysarthria absent.
Rebound phenomenon absent.
Intentional tremors - absent.
Pendular knee jerk - absent.
Tandem walking normal.
Coordination tests
Dysdiadochokinesia absent
Finger nose test normal
Heel knee test normal
Rombergs Test - Negative
Micrographia +
✓This is a test to elicit the bradykinesia component of Parkinson's disease.
✓Findings - The movements in the right lower limb is slower than the movements in the left lower limb.
✓The first test was only toe tapping, the second test is entire foot tapping.Rapid supination and pronation - Diadochokinesia
✓MENINGEAL SIGNS
Neck stiffness - Absent
Kernig's sign - Negative
Brudzinski's sign - Negative
✓AUTONOMIC
Postural hypotension+(Supine - 180/110, Standing 160/90).
Resting tachycardia absent(PR 80/min, regular)
Abnormal sweating absent.
H/O erectile dysfunction+.
Cardiovascular System
S1, S2 +.
Apex beat in 5th ICS on the MCL.
JVP normal.
✓ Shows Sinus Tachycardia with pseudo infarct pattern in leads I and aVL with dagger q waves in the same leads.
✓ No late intrinsicoid deflection of R wave with modified Cornell criteria showing LVH.
2 D Echo
✓ Grade II diastolic dysfunction.
Respiratory System
Shape & symmetry of chest - Normal
Respiratory movements - Equal on both sides
BAE+
NVBS
Abdominal Examination
Soft, Non-tender
No organomegaly
Bowel sounds+
Problem Representation -
A middle aged man presenting with a 6 months history of gradually progressive, asymmetric rest tremor with autonomic features is provisionally diagnosed with
1. Idiopathic Parkinson's Disease Stage 1 with denovo HTN.
2. Multiple System Atrophy - Parkinsonian Type (MSA-P).
Treatment
1. Tab. Syndopa Plus 125 mg QID
2. Tab. Syndopa 125 mg CR OD
3. Tab. Telma 40 mg O
SHORT CASE-2:
19 year old male resident of Nalgonda and currently studying intermediate, came to OPD with complaints of:
-Itchy Ring leisons over arms, abdomen, thigh and groin since 1 and half year.
-Purple stretch marks all over abdomen, lower back, upper limbs, thighs since 1 year.
-Abdominal distension and facial puffiness since 6 months.
- Pedal edema since 3 months.
- Low back ache since 3 months.
- Feeling low, not feeling to talk to anyone.
- Weight gain and decreased libido since 3months.
- Loss of libido and erectile dysfunction since 2 months.
Pt was apparently alright one and half year ago, when he slowly developed erythematous round leisons which are annular shaped and itchy all over abdomen, upper limb, groin and inner thigh region.
No history of fever back then. No other complaints apart from skin lesions.
Pt visited local RMP where he prescribed auyurvedic medications and other creams ( unknown composition as pt don't have them currently). He also prescribed tablets (unknown composition). Patient started using all these medications for 1-2 months.
Leisons reduced a bit after using medications.
Later after 2 months he developed multiple hyper pigmented plaques over lower limbs abdomen, for which he again visited same place and used ayurvedic oils over the leisons.
He also used clobetasol ointment over the leisons. (for approximately 1 year all over the body)
He started noticing pink striae over his abdomen first and later on back and over arms, which were gradually increasing in size.
Later he visited a hospital and used miconazole and luliconazole ointments also.
He used clobetasol ointment all over the leisons for long time.
He started noticing abdominal distension and facial puffiness, weight gain, but never visited any hospital.
Later he developed pedal edema and low back ache since 3 months .
His consulted a dermatologist at this point of time who advised to consult physician and prescribed monteleukast, itraconazole tablets, luliconazole ointment for tenia corporis.
He stopped all medications one month ago and visited our opd with complaints of pink striae and easy fatigue, weakness and low back ache.
His brother also gave history of pt being moody and feeling of low self esteem due to multiple leisons.
He even complaints pt wouldn't step out of house and always stays indoor and wouldn't interact with others.
No complaints of chest pain, sob, palpitations.
No complaints of decreased or frothy urine.
No other negative history.
No h/o DM, HTN, TB, ASTHMA, CAD.
ALLERGIC HISTORY - pt gives h/o allergy to eggs, brinjal.
O/E: Pt was c/c/c
BP - 160/100 mmHg
Pr - 96 BPM, regular ,normovolemic .
Rr - 18/min
Spo2- 98% on ra.
Weight - 63 kg.
Height - 175 cm.
GENERAL EXAMINATION:
NO pallor, icterus, cyanosis, clubbing, lymphadenopathy.
Pedal edema present - pitting type extending upto knee.
Abdominal distension present.
Moon face present
Pink striae noted over anterior abdominal wall and on low back and on upper arms and thighs.
Thin skin present.
Poor healing noticed over leg ulcers and easy bruising noted.
Acne present over face.
Acanthosis nigrans noted over neck.
GYNECOMASTIA PRESENT.
Buffalo hump present.
Sparse scalp hair.
Skin examination - Multiple itchy erythematous annular leisons noted all over abdomen, upper limb, groin and inner thigh region.
Multiple hyperpigmented plaques noted over bilateral lower limbs.
SYSTEMIC EXAMINATION:
CVS - S1S2 heard. No murmurs
RS - BAE present.
No adventitious sounds.
P/A - Soft, distended.
No organomegaly.
Bowel sounds present.
CNS - HMF - INTACT R. L
MOTOR SYSTEM - POWER - UL 5/5 5/5
LL 5/5 5/5
Proximal muscles lower limb - power is 4/5.
TONE - NORMAL.
REFLEXES - B. T. S. K. A. P
R. +2 +2. +1. +2. +1. FELXOR
L. +2. +2. +2. +2. +1. FLEXOR.
CRANIAL NERVES - NORMAL.
Difficulty in getting up from chair was noticed.
PROVISIONAL DIAGNOSIS -
? IATROGENIC CUSHINGS SYNDROME .
TINEA CORPORIS.
DENOVO HTN .
INVESTIGATIONS:
CBP - HB - 13.4 g/dl
TLC - 6,800
PLT - 1.5 lakhs.
RBS - 139 mg/dl
CUE - ALBUMIN - +1
SUGARS - NIL.
PUS CELLS - 3-4
RBC - NIL.
LFT - TB -1.03
DB-0.21
ALBUMIN - 3.9
RFT - UREA - 22
SERUM CREATININE -0.6
ELECTROLYTES - NA - 136
K- 4
CL-98
USG ABDOMEN - NORMAL.
ECG - SINUS TACHYCARDIA
LVH PRESENT.
This was picture of striae one year ago when it gradually started:
On presentation to opd pictures: 28/05/21
We took dermatologist opinion for tenia corporis where they advised
Ointment AMLORFINE
FUSIDIC ACID CREAM.
SALINE COMPRESS OVER LEISONS.
Plan to start anti fungals on next visit once dose of steroids is reduced .
OPTHAL opinion Was taken to look for visual acuity and cataract.
No features of lens opacities noted.
BUT IOP was high, where they advised to follow up.
We advised pt to get fasting 8am serum cortisol levels and was planned to start on low dose steroids to avoid adrenal crisis.
8AM S CORTISOL LEVELS (30/5/21)
- 0.46 mcg/dl (very low).
(normal range - 4.3-22.4 mcg/dl).
In view of lvh pt was started on tab telma 20 mg od.
On 3/6/21 - ACTH STIMULATION TEST WAS DONE.
BY INJECTING 0.4 ML OF ACTOM PROLONGATUM INJECTION (ACTH) INTRA MUSCULAR @ 7am
1 HR LATER FASTING SERUM CORTISOL SAMPLE WAS SENT.
VALUE - 0.73 mcg/dl
Indicating there was HPA AXIS suppression and pt was started on TAB HIZONE 15 mg per day in three divided doses @ 8am ,12 pm and 4 pm.
Pt was asked to follow up after one month .
ON NEXT VISIT: (25/6/21).
Pt was symptomatically better, pedal edema subsided.
Striae were pale in color and we're subsiding.
Weight - 67kg
Ht -175 cm.
Bp- 160/100 mmHg.
Pr -88bpm.
Dose of Tab hizone was reduced to 10 mg per day in divided doses for one month.
In view of low back ache Xray LS spine was done which was normal and pt was advised.:
Tab Shelcal 500 OD and Tab Vit D 3 Od.
Tab ULTRACET /PO/SOS.
Psychiatry opinion was taken and he was diagnosed with moderate depression.
In July 2021 pt was complaining of fever, sore throat and dry cough since 3 days and he was tested positive for COVID 19, we advised him home isolation and PCM 650 Mg /po /sos .
He was advised to continue tab hizone tablets as it was advised.
He recovered within one week.
Next visit: (6/8/21).
BP- 170/100 - TELMA DOSE WAS INCREASED TO 40 MG OD.
PR - 88bpm. regular, normovolemic.
Wt- 69 kg
Height -
Abdominal girth - 96cm
Pt complaints of excoriation over striae and appearance of erythematous macules over abdomen whenever he takes food he is allergic to.
Took dermatologist opinion for it. They started him on Tab Itraconazole 100 mg bd. And lulifin cream and tab levocitrixine 5mg od.
His brother complaints of depressed mood, pt not going out due to social stigma. Psychiatric counselling was given.
He still complaints of low back ache.othropedics opinion was taken and advised to continue Ultracet and tab Shelcal .
Cbp , cue and electoltes were repeated which were all in normal range.
USG ABDOMEN was done - Normal kidney size bilateral and CMD maintained. No other sonological abnormality noted.
As his lesions dint subside we reduced dose of hisone to 7.5 mg per day, to see response.
At this point of time we are now in diagnostic dilemma whether endogenous CUSHINGS is also present in this patient, as he is responding slowly to treatment.
We advised him to review after 15 days to see progress . And accordingly plan to evaluate further to rule out endogenous CUSHINGS SYNDROME.
FINAL DIAGNOSIS:
IATROGENIC CUSHINGS SYNDROME SECONDARY TO TOPICAL CLOBETASOL APPLICATION ALL OVER BODY FOR APPROXIMATELY ONE YEAR.
TINEA CORPORIS
DENOVO HTN.
THESIS
AUGUST 09, 2021
TITLE
“ASYMPTOMATIC LEFT VENTRICULAR (LV) DIASTOLIC DYSFUNCTION IN PATIENTS OF TYPE 2 DIABETES MELLITUS OF 1 TO 10 YEARS DURATION”
INTRODUCTION
In the year 2000, India topped the world with the highest number of people with Diabetes Mellitus with 31.7 million people affected with it, giving it a status of a potential epidemic. [1] In 2014, this figure more than doubled to 62 million of the adult population diagnosed with Diabetes. According to Wild et. al. this figure may reach nearly 80 million by the end of 2030,
further establishing its status as a potential epidemic. [2] According to the recently conducted National Family Health Survey,
(NFHS-4, 2015-16) 6.3% of adult women in Nalgonda suffer from Diabetes Mellitus, with Khammam having the highest prevalence at 7.6% of its adult population. [3] Left ventricular diastolic dysfunction in asymptomatic patients with diabetes mellitus may represent the early stage of diabetic cardiomyopathy even in patients without structural cardiac disease or systemic hypertension and have a preserved left ventricular systolic function. [4] Diabetic cardiomyopathy was first reported by Rubler et al. [5] in 1972 when they described four diabetic patients with heart failure, normal coronary arteries, and without obvious aetiology for heart failure and stated that it was due to diabetic cardiomyopathy.
Studies have reported a high prevalence of pre-clinical LV diastolic impairment in diabetic patients [6] and this cardiac complication may represent the reversible early stage of heart failure which is termed diabetic cardiomyopathy. Cardiac involvement in patients with diabetes mellitus may occur relatively early in the course of disease, impairing left ventricular (LV) relaxation (diastolic dysfunction) and later on can affect ventricular contraction (systolic dysfunction). [6]
AIM
To Study Asymptomatic Left Ventricular (LV) diastolic dysfunction in patients of Type 2 Diabetes Mellitus of 1 to 10 years duration.
OBJECTIVES
To study asymptomatic diastolic dysfunction in patients with Type 2 Diabetes Mellitus.
RESEARCH QUESTIONS
1. Is there a correlation between glycaemic control and grade of diastolic dysfunction?
2. Does duration alone affect the grade of diastolic dysfunction?
3. Does grade 3 diastolic dysfunction (restrictive filling pattern) occur in diabetics of less than 10 years duration?
METHODOLOGY – PATIENTS AND METHODS
PATIENTS: Type 2 Diabetes Mellitus patients (insulin dependent or non-dependent), that are free from cardiac symptoms (e.g., exertional Dyspnea, Angina) with duration between 1-10 years, of out-patients or in-patients admitted in Medical wards or ICU in KIMS, Narketpally.
✓ STUDY DURATION: Recruitment of patients would begin from
October 2018 - September 2020.
✓ STUDY DESIGN: Qualitative, Cross-sectional, Exploratory
✓ SAMPLE SIZE: 60
✓ INSTITUITIONAL ETHICAL COMMITTEE CLEARANCE & PATIENTS OFFERING VOLUNTARY WRITTEN INFORMED CONSENT TO PARTICIPATE IN THIS STUDY
INCLUSION CRITERIA
1. Age >40 years
2. Patients diagnosed with Type 2 Diabetes Mellitus of 1 to 10 years duration.
EXCLUSION CRITERIA
1. Patients with CAD diagnosed by symptoms, ECG or regional wall motion abnormalities on echocardiogram or prior coronary angiography.
2. Patients with heart failure diagnosed by signs and symptoms, chest radiograph or echocardiography.
3. Patients with significant valvular heart disease, diagnosed clinically or with echocardiography.
4. Heart rate <50 or >100 beat per minute, atrial fibrillation and other
arrhythmias that may interfere with Doppler studies.
5. Hypertensive patients (Either a known case on treatment or when
blood pressure is greater than 140/90 mmHg) [7]
6. Patients with long history of diabetes mellitus (>10 years) or duration of < 1 year.
7. Subjects with poor transthoracic echocardiographic window.
STUDY PROTOCOL
This study will include all patients of Type 2 Diabetes Mellitus, greater than 40 years of age falling into criteria set by American
Diabetic Association. [8]
All patients will be subjected to the following investigations:
i. Hemogram
ii. Complete Urine Examination
iii. Diabetic Profile – FBS, PPBS. HbA1c
iv. Blood Urea, Serum Creatinine and Serum Electrolytes
v. Fasting Lipid Profile
DIAGNOSTIC CRITERIA FOR TYPE 2 DIABETES MELLITUS
Fasting blood sugar (FBS) ≥ 126 mg/dL
(or)
Post-prandial blood sugar ≥ 200 mg/dL
(or)
HbA1c ≥ 6.5% or Classic diabetes symptoms + random plasma glucose
≥ 200 mg/dL
DIAGNOSTIC CRITERIA USED IN 2D-ECHOCARDIOGRAPHY
Subjects will be examined using standard parasternal long axis, short axis and apical two and four chambers views. Conventional techniques (two-dimensional-2D, M-mode echocardiography, Pulsed-wave Doppler wave (PW) and TDI methods will be used for
1. LV internal dimensions: LV end systolic dimension (LVESD) and LV end diastolic dimension (LVEDD).
2. Ejection fraction (EF %) (Using Teichholz method).
3. E point (m/sec): Early diastolic velocities of mitral inflow (Doppler-derived).
4. Septal and lateral e point by tissue Doppler (m/sec): Early diastolic myocardial velocity, derived from tissue Doppler imaging.
5. E/e ratio: Ratio of early diastolic velocities of mitral inflow (PW-derived) and myocardial movement (TDI-derived) taken as left ventricular filling pressure.
6. Left atrial (LA) volume index (mL/BSA): In apical four and two-chamber views.
7. Peak tricuspid regurgitation (TR) velocity (m/sec). Systolic dysfunction was defined if LV Ejection fraction <50%.
DEFINITION OF LV DIASTOLIC DYSFUNCTION
Definition of LV diastolic dysfunction will be indicated if 3 or more of these variables are abnormal:
→ Septal e <7 cm/sec
→ Lateral e <10 cm/sec
→ E/e ratio >14
→ E/A ratio < 0.8
→ LA volume index >34 mL/m2
→ Peak TR velocity >2.8 m/sec.
Diastolic dysfunction will be divided into three grades :
• Grade I; impaired LV relaxation.
• Grade II ; pseudonormal filling pattern.
• Grade III ; restrictive filling pattern.
PARAMETERS USED FOR DATA ANALYSIS
The parameters used will be categorised separately for men and women.
→ Age
→ Duration
→ Body Mass Index (BMI)
→ Haemoglobin A1c (HbA1c)
→ E/A ratio
→ E/e ratio
→ Left Atrium Size (LA Volume Index)
→ Tricuspid Regurgitation Velocity (TR Velocity)
→ Left Ventricular Ejection Fraction (LVEF / EF)
→ Diastolic Dysfunction
* p value <0.05 is considered statistically significant and p value
<0.001 is considered highly significant.
LOG BOOK
AUGUST 09, 2021
LOG BOOK
MAY 2020
JUNE 2020
JULY 2020
AUGUST 2020
SEPTEMBER 2020
OCTOBER 2020
NOVEMBER 2020
DECEMBER 2020
CORE CLINICAL COMPETENCIES
AUGUST 09, 2021
Core clinical competencies:
A few selected procedural skills videos -
Clinical Discussions and Presentations - A few selected videos are shared in the playlist below -
Demonstration of Interesting Clinical Signs and a few learning points on Echocardiography
HALLTICKET NO. 18100006004
CASES.
LONG CASE:
AUGUST 09, 2021
CASE PRESENTATIONS
26 year old male, construction worker by occupation presented to the casualty with the chief complaints of
Fever since 3 months





 The World Health Organization estimated that there were 463 million diabetics in 2019 and this number would increase to 578 million by the year 2030 and 700 million by 2045. India leads the world with largest number of diabetic subjects earning the dubious distinction of being termed the “Diabetes capital of the world”. (1) According to the Diabetes Atlas 2017 published by the International Diabetes Federation, the number of people with diabetes in India currently around 72.9 million is expected to rise to 134.3 million by 20453. Diabetic nephropathy is one of the leading causes of chronic renal failure in India. DIABETIC RETINOPATHY: In India, the previous studies to calculate prevalence were by Raman et al. (18.1%) (4), Rema et al. (17.%) (5), Namperumalsamy et al. (10.6%) (6), Narendran et al. (26.2%) (7) and Dandona et al (8). The prevalence in the AIOS study was 21.27% with a range of 12.27% in the central zone and 34.06% in the north zone.PERIPHERAL VASCULAR DISEASE: Prevalence of PAD in T2D patients in Delhi, North India, is much lower than that reported in western population (∼20%) and from south India (6.3%). Prevalence of PAD was higher in patients with higher age, longer duration of diabetes, lower BMI, and higher total and LDL cholesterol (9). CORONARY ARTERIAL DISEASE: The prevalence of CAD in the CUPS study was 11% in the total population, with 1.2% patients having had a MI, 1.3% with Q-wave changes, 1.5% with ST-segment changes, and 7.0% with T-wave abnormalities (10,11). This 11% represents a 10-fold increase in CAD prevalence in urban India since 1970 (10,12), now approaching those reported in migrant Indians. In the same study, the prevalence of CAD among diabetic subjects was 21.4% (known diabetes, 25.3%, and newly diagnosed diabetes, 13.1%), which was much higher than the figure of 14.9% among subjects with IGT and 9.1% among those with NGT. Prevalence of known MI was three times higher in diabeticsubjects. DIABETIC NEPHROPATHY: A study was performed to evaluate the various etiologies of CKD among patients presenting to the Department of Nephrology, Guwahati Medical College, a tertiary referral center. A total of 5718 CKD patients were evaluated to identify the cause of CKD. The most common cause was found to be diabetes mellitus in 42.2%, followed by chronic glomerulonephritis in 21.4%, hypertension in 19.5%, obstructive uropathy in 6.9%, chronic interstitial nephritis in 3.6%, and autosomal dominant polycystic kidney disease in 1.5% of the patients. Nearly 2.7% of the patients had CKD of unknown etiology (13). EFFECT OF SOCIOECONOMIC STATUS Prevalence of diabetes was found to be lower in low socioeconomic group living in urban areas compared with the high income group. This was probably related to the physical activity of the low income group as most of them were involved in moderate to strenuous physical activity. However long term complications like CAD, CKD, PAD and diabetic retinopathy are more common in low socioeconomic group because of uncontrolled blood sugars, alcohol and smoking.
The World Health Organization estimated that there were 463 million diabetics in 2019 and this number would increase to 578 million by the year 2030 and 700 million by 2045. India leads the world with largest number of diabetic subjects earning the dubious distinction of being termed the “Diabetes capital of the world”. (1) According to the Diabetes Atlas 2017 published by the International Diabetes Federation, the number of people with diabetes in India currently around 72.9 million is expected to rise to 134.3 million by 20453. Diabetic nephropathy is one of the leading causes of chronic renal failure in India. DIABETIC RETINOPATHY: In India, the previous studies to calculate prevalence were by Raman et al. (18.1%) (4), Rema et al. (17.%) (5), Namperumalsamy et al. (10.6%) (6), Narendran et al. (26.2%) (7) and Dandona et al (8). The prevalence in the AIOS study was 21.27% with a range of 12.27% in the central zone and 34.06% in the north zone.PERIPHERAL VASCULAR DISEASE: Prevalence of PAD in T2D patients in Delhi, North India, is much lower than that reported in western population (∼20%) and from south India (6.3%). Prevalence of PAD was higher in patients with higher age, longer duration of diabetes, lower BMI, and higher total and LDL cholesterol (9). CORONARY ARTERIAL DISEASE: The prevalence of CAD in the CUPS study was 11% in the total population, with 1.2% patients having had a MI, 1.3% with Q-wave changes, 1.5% with ST-segment changes, and 7.0% with T-wave abnormalities (10,11). This 11% represents a 10-fold increase in CAD prevalence in urban India since 1970 (10,12), now approaching those reported in migrant Indians. In the same study, the prevalence of CAD among diabetic subjects was 21.4% (known diabetes, 25.3%, and newly diagnosed diabetes, 13.1%), which was much higher than the figure of 14.9% among subjects with IGT and 9.1% among those with NGT. Prevalence of known MI was three times higher in diabeticsubjects. DIABETIC NEPHROPATHY: A study was performed to evaluate the various etiologies of CKD among patients presenting to the Department of Nephrology, Guwahati Medical College, a tertiary referral center. A total of 5718 CKD patients were evaluated to identify the cause of CKD. The most common cause was found to be diabetes mellitus in 42.2%, followed by chronic glomerulonephritis in 21.4%, hypertension in 19.5%, obstructive uropathy in 6.9%, chronic interstitial nephritis in 3.6%, and autosomal dominant polycystic kidney disease in 1.5% of the patients. Nearly 2.7% of the patients had CKD of unknown etiology (13). EFFECT OF SOCIOECONOMIC STATUS Prevalence of diabetes was found to be lower in low socioeconomic group living in urban areas compared with the high income group. This was probably related to the physical activity of the low income group as most of them were involved in moderate to strenuous physical activity. However long term complications like CAD, CKD, PAD and diabetic retinopathy are more common in low socioeconomic group because of uncontrolled blood sugars, alcohol and smoking.