HALL TICKET NO. 1800006009
Informant: Patient
A 38 year old male, a resident of Chandanapally, Nalgonda district came to the hospital with complaints of difficulty in walking since 8 years
Chief complaints: difficulty in walking since 8 years (2014 March)
Feeling weak during walking since 7 years (2015 January)
History of present Illness: The patient had difficulty while walking, while getting up from chair without support, but gets up from chair with support, difficulty in squatting, difficulty in sitting on floor, difficulty in getting up without support from floor.
Initially he had difficulty in going uphill but since 3 years he was complaining of difficulty in walking on level ground also.
Uphill: steps are difficult
Downhill: comparatively easier steps than uphill
Difficulty in running
The patient did not have any difficulty in wearing chappals, holding chappals. He did not have any problem in removing chappals. However he complained that it was easier to walk without chappals since there was lesser weight lifting needed.
After having these symptoms for 8-9 months the patient went to the hospital for checkup and was given medication for which there is no record of with the patient. According to the patient, he was not on regular medication and the medication didn’t improve his symptoms.
Overtime, he had feeling of heaviness of upperlimb while lifting his hand over the head which progressed over time to having difficulty in lifting his arm to shake hands, eat his food and take his brush from the cupboard. He complains that he has to give an increased initial try for him to lift his hand.
After initiating combing, he doesn’t have any difficulty in combing the hair. He feels that it is difficult to move the brush in his mouth.
Difficulty in lifting food to mouth. Not associated with falling of food particles and not associated with falling of food from mouth. No difficulty in chewing food after putting food in the mouth.
Difficulty in bathing with mug. Washes more on the right side with difficulty in washing on the left side.
Difficulty in getting from bed without support since 1 year. No difficulty in turning to sides on bed.
No difficulty in eating, chewing, closing eyes, swallowing food, whistling, shouting, winking.
Complaints of intermittent spasm of muscles after prolonged sitting. Complaints of muscle cramps.
No complaint of difficulty in feeling things he touches. No difficulty in feeling chappals sensation. As he walks without chappals he is used to pain while walking and says that his feet are more prone to injuries.
He doesn’t have any difficulty in feeling pain when there is an injury. He doesn’t have ulcerations or abnormal sensations anywhere on the body.
He is able to feel the temperature of the water while bathing.
The patient doesn’t have any complaints of blurring of vision, difficulty in smell, double vision, vision difficulties, no loss of area of vision, no difficulty in swallowing and tasting, normal facial expressions, no difficulty in hearing sounds of low intensity or high intensity.
No difficulty in turning head, no difficulty in eating or drinking.
No history of loss of consciousness, no irritability to light or sound, no loss of memory, no abnormal visions, sounds, the patient does not use spectacles.
The patient complains the he feels bad that he lost his job as a watchman because of the difficulty in working after onset of difficulty in walking and weakness. But he does not have history of acting out. He feels bad about not earning money but he tells that he got used to the complaints over time.
No history of headaches, nausea, vomiting, involuntary movements.
The patient does not complain of loss of balance or falls but he tells that sometimes while getting up from a chair, he doesn’t have the power to get up and sits back.
No complaints of urgency, hesitancy, increase in frequency during night, difficult in initiating urination, burning during urination.
He had complaints in difficulty in passing stools intermittently for which he takes more water or a tablet and the symptom subsides. He didn’t contact doctor for the complaint as it was intermittent and reduced with more intake of water and bananas.
No history of fever, sleep disturbances, no history of injury to feet.
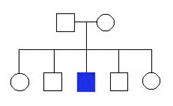
Birth history: The patient had history of second degree consanguinity and was born at home with the help of dai and apparently without any problem after birth in his words.
He walked without support at 3 years and started talking in sentences at 7 years of age. He has stuttering while talking but doesn’t have a problem in formation of sentence, language or difficulty in pronunciation of words. He says that he stutters more when there is lack of sleep.
Family history: No history of similar complaints in the family. His mother and father died in an accident and he is not married due to his stuttering problem at first and weakness later.
Personal history: The patient was a smoker previous for 6 months in 2012 but stopped later.
He is an occasional alcoholic and drinks one glass of toddy during festivals. No sleep and appetite abnormalities. No bowel and bladder abnormalities.
Past history: The patient had a history of fall from cycle in 2012 after which he had a fracture in the left wrist but did not go to the hospital and took Ayurveda treatment. Now there is a deformity in the left wrist and reduced range of movement with difficulty in using the hand.
No known history of diabetes, hypertension, bronchial asthma, allergies, tuberculosis, jaundice or prolonged hospital stay.
Drug history: No known usage of drugs for more than 1 week, no history of usage of injections in the hospitals. No known history of any drug allergies.
Summary: Based on the above history the patient had slowly progressive weakness of the lower limbs more proximal than the distal and overtime it progressed to the upper limbs with more proximal weakness than distal and he developed weakness in the trunk overtime. He doesn’t have spasticity or rigidity in the muscles. He doesn’t have sensory complaints. He complains weakness more in the lower limbs than upper limbs. He has no cerebellar, autonomic system, cranial nerves or higher mental function abnormalities. The patient had history of consanguinity, delayed milestones and history of malunited left wrist fracture.
General physical examination: The patient is conscious, coherent, comfortable, cooperative. No distress or features of pain. The patient doesn’t appear pale.
There is no icterus, clubbing, cyanosis, pedal edema, generalised lymphadenopathy on examination.
Weight- 54 kgs
Height- 162 cms
BMI- 20.57 kg/m2
BP- 110/70mm Hg
Hair, nails, skin and spine- normal
Systemic examination:
Neurological examination:
Higher mental functions: The patient is conscious, appears comfortable, language and behaviour appears normal.
Orientation to time place and person normal. Mood and emotional status appears normal.
Memory: immediate, recent and remote memory tested- normal.
Mini mental status examination score- orientation-5/5
Registration-3/3
Attention and calculation- 2/5
Recall- 3/3
Total score- 25/30
No illusions or hallucinations
Speech: normal verbal output, fluency, repetition, naming, reading, writing.
Appearance- no tics, tremors, myoclonus, involuntary or voluntary movements
Motor examination:
Bulk:
upper limb- right upper limb- 24.5 cms above elbow, 22cms below elbow
Left upper limb- 23.5cms above elbow, 22 cms below elbow
Lower limb- right lower limb- 43 cms above knee, 32 cms below knee
Left lower limb- 43 cms above knee, 32 cms below knee
Tone: hypotonic in right upper limb and lower limb, hypotonic in left upper limb and lower limb.
Power: Right Left
Upper limb- distal flexors- -4/5 -4/5
Proximal flexors 3/5 3/5
Hand muscles- extensor pollicis longus- 3/5 on both sides, all the others are 4/5 power
Trunk muscles- 3/5 on both sides
Lower limb- hip muscles- iliopsoas- 3/5 on both sides
Adductor femoris- 3/5 on both sides
Hamstring muscles- 3/5 on both sides
Gastrocnemius muscles- -4/5 on both sides
Extensor hallucis longus- -4/5 on both sides
Coordination- normal coordination of movements
Reflexes: biceps- reduced but present + on both sides
Supinator- + on both sides
Triceps- + on both sides
Ankle - + on both sides
Plantar- flexor response on both sides
Sensory examination:
Touch- normal on both sides
Temperature- both hot and cold sensation normal on both sides
Vibration- normal on both sides
Joint position- 5/6 times on right side, 6/6 times on left side
Cerebellar examination:
Hypotonia- present
No rebound phenomenon
Finger nose test- normal
Finger finger test- normal
Heel shin test- normal
No past pointing, intentional tremor or gait abnormalities.
Gait: normal stride, Normal width, normal turning, the patient is not able to walk on toes.
Cranial nerves: normal smell and vision
Pupillary light reflex- normal, accommodation reflex - normal, normal manual perimetry, normal primary eye movements, normal sensations over the face, normal glabellar tap, corneal reflex, conjunctival reflex and jaw jerk, normal facial expressions, normal taste sensations all over tongue, no deviation of facial muscles or tongue muscles. Normal shrugging, head turn against pressure.
Autonomic system: no bowel bladder abnormalities, no abnormal sweating, no orthostatic hypotension, no postprandial syncopal attacks, no history of falls with loss of consciousness.
Intracranial pressure: no signs of raised intracranial pressure
Skull and spine: normal
Cardiovascular system:
Inspection: normal on inspection, no visible pulsation, apex beat not visualised. No visible lesions on chest. Equal and symmetrical chest movements with respiration.
Palpation: apex beat felt on the left 5th intercostal space 1cm medial to mid clavicular line. All the findings of inspection are confirmed.
Percussion- all the borders of heart normal on percussion
Auscultation- s1, s2 heard.
No added sounds, no murmurs heard, normal split heard in s2.
Respiratory system:
Inspection- normal on inspection, no visible pulsation, apex beat not visualised. No visible lesions on chest. Equal and symmetrical chest movements with respiration.
Palpitation- apex beat felt on the left 5th intercostal space 1cm medial to mid clavicular line. All the findings of inspection are confirmed.
Percussion- no abnormal findings on percussion
Auscultation- normal vesicular breath sounds heard equally on both sides
Abdominal examination:
Inspection- normal on inspection, no visible pulsations, no visible lesions on abdomen.
Palpation- no organomegaly
Percussion-
Auscultation- bowel sounds heard at normal frequency
ECG -
Chest X-ray- normal

Serum creatine phoshokinase- 780 IU/ lit
Nerve conduction study- normal
Elctromyography- reduced amplitude with polyphasic motor response- suggests myopathy
Muscle biopsy report-

Final diagnosis: Based on the above history, examination and findings, the most probable diagnosis is progressing symmetrical proximal muscular dystrophy involving both lower limbs and upper limbs without any known family history or heart involvement so most probably could be beckers or limb girdle muscular dystrophy based on the above mentioned findings.
Differential diagnosis- the other possible diagnosis could be chronic inflammatory demyelination syndrome but it is predominantly sensory and in this case sensory findings are minimal.
Other possible diagnosis could be proximal motor neuropathy or neuronopathy but there is no history of diabetes or involvement of muscles of neck, swallowing.-------------------------------------------------------------------------------------------------SHORT CASE-1:
Informant: patient’s daughter
A 58-year-old woman presented with the complaints of
Chief complaints: Shortness of breath with exertion since 1 year and at rest since 15 days
Cough intermittently since 4 months
Swelling of both lower limbs on and off since 2 months
Swelling of right lower limb since 10 days
History of present illness: the patient had complaint of shortness of breath since 1 year which was present with farm work started insidiously, progressing over time, exertional, non seasonal, reached the present state of shortness of breath at rest. Associated with increase during sleeping position and relieved during sitting or standing position.
Complaint of cough with expectoration intermittently, associated with worsening of chest pain, not associated with fever, no diurnal variations. Expectorant- whitish to slightly pinkish in colour, not foul smelling, no plugs, no frank blood.
Complaint of bilateral pedal edema on and off since 2 months, pitting present, extending till ankles, equal on both sides.
Not associated with chest pain, dizziness, loss of consciousness, abnormal sensations of heart beat.
Not associated with fever, loss of weight.
Associated with increased frequency of urination since 4 months
Past history: No history of similar complaints before 1 year. History of hospitalisation for 3 times in the past one year. Episodes of hospitalisation associated with worsening of shortness of breath, pedal edema and cough. Each time the patient’s attenders gave history of on and off medication intake.
No history of diabetes, hypertension, bronchial asthma, tuberculosis, jaundice.
No known drug allergies.
Family history: no history of similar complaints in the family. No history of sudden cardiac death in the family.
General physical examination: The patient appears conscious, cooperative, dyspnoea at rest present.
Pulse- rate 86 beats per min
Rhythm- regular, volume- low volume, equal pulses on both sides and in all peripheral areas, no radio radial delay, no radio femoral delay.
Blood pressure- 120/60mm Hg
Jugular venous pressure- engorged vein, pulsation, the patient has hepatojugular reflex
Respiratory rate - 24 cycles per minute
Spo2 - 96% on room air
Pallor- present, no icterus, cyanosis, clubbing, lymphadenopathy.
Pedal edema- present, bilateral pitting type, extending till ankles.
Cardiovascular examination:
Inspection:
No deformity or bulge in the precordium, apical impulse seen in sixth intercoastal space 1cm lateral to the midclavicular line, no diffuse pulsations over precordium, no superficial engorged veins. No scars or sinuses over the skin.
Pulsations seen on the right parasternal region and in the epigastrium.
No prominent pulsations in the aortic, suprasternal area, supraclavicular area, no visible carotid pulsation, no visible pulsations on the back.
No kyphosis, scoliosis, drooping of shoulder, winging of scapula.
Palpation:
Apex beat present in the 6th inter coastal space, left sided, 1cm lateral to the midclavicular line over 2 inter coastal spaces. Parasternal heave present on the right parasternal region, obliterated on pressure.
Palpable second heart sound in the pulmonary area, not associated with palpable thrill in the pulmonary area.
No other palpable heart sounds, no thrill in carotid pulse, no superficial veins.
Percussion- right border of heart- dull ness on percussion seen till 2.5 cms lateral to the sternal border. Other borders not well localised.
Auscultation:
cardiac rate- about 87 beats per minute
Regular in rhythm
Mitral area- soft s1 heard, associated with diastolic murmur mid to late low pitched, no presystolic accentutation, more heard on the left lateral position. No radiation of the murmur heard.
Difficult to appreciate when the patient initially came to the hospital but better audible after initial management.
Pulmonary area- loud p2 heard, no murmur heard, no added sounds
Aortic area- s2 with normal split heard, no murmurs or added sounds heard
Tricuspid area- no murmurs or added sounds heard
Provisional diagnosis- based on the above history and examination the most probable diagnosis is moderate to severe mitral stenosis with frequent acute exacerbations of heart failure.


-------------------------------------------------------------------------------------------------
SHORT CASE-2:
Informant- patient
Chief complaints: A 54 year old male patient came with Pain in the left side of the chest radiating to the back side since 8 days, difficulty in breathing since two days.
History of present illness: Patient was apparently asymptomatic 8 days back then he developed pain in the left side of chest all over, of stabbing type, which increased on inspiration, radiating to the left upper back.
Pain associated with difficulty in breathing with pain during inspiration, progressing over time, increased with intermittent cough.
Not associated with high grade fever, chills.
No history of shortness of breath before 8 days.
No history of palpitations orthopnoea, PND, headache, burning micturition, vomiting loose stools, cough, fever.
No history of headache, tingling sensation, numbness.
No history of decreased urine output.
History of burning sensation of both feet since 1 year, associated with tingling sensation of both lower limbs extending till ankle, equal on both sides, difficulty in feeling chappals while walking.
Past history:
The patient has reduced vision in the right eye post trauma and also sustained a leg injury during trauma after which he started using a stick to assist his walking.
He was also operated 10 years back due to a mass in the scrotum (? Inguinal hernia)
There is no history of Hypertension, Diabetes mellitus, epilepsy, bronchial asthma, coronary artery disease.
Family history: no history of similar complaints in the family
Personal history: The patient is a chronic alcoholic and consumes about 180ml of alcohol per day, 4-5 days per week. Not a known smoker. Married and has 2 kids.
General physical examination: On Examination the patient was in sitting position, conscious coherent and cooperative.
Febrile to touch- 99.3F
Pulse- 98 beats per minute, regular, normal volume, no radio radial or radiofemoral delay
BP 120/100mmHg
No pallor, icterus, clubbing, lymphadenopathy, pedal edema
Spine appears normal
Respiratory examination:
Upper respiratory tract: nose, septum, sinuses, oral cavity and pharyngeal cavity normal.
No mouth breathing.
Lower respiratory tract:
Inspection: The patient is sitting in proper light and was examined. Shape appears to be elliptical. Movements of chest slightly reduced on the left side of chest. Apical impulse not visible. Abdominal type of respiration. About 19 cycles per minute. No visible deviation of trachea. No visible veins or pulsations. No scars, marks or sinuses. Inter coastal fullness present on the left side localised to the lower half. No accessory muscle usage. Normal nipples and muscles on inspection. No audible sounds. No shoulder or spine abnormalities on inspection.
Palpation: Normal surface temperature. No local tenderness. No deviation of trachea. Reduced chest movement on the left side. No spinal or shoulder deformity. Asymmetrical chest expansion seen with reduced movements on the left side. Reduced vocal fremitus in the left infrascapular and left infraaxillary region.
Percussion: Stony dull note on percussion in the left infrascapular region and left infraaxillary region. Normal resonant note in all the other areas.
Auscultation: Bilateral air entry present. Equal sounds on both sides. Normal vesicular breath sounds in right infraclavicular, clavicular, supraclavicular, mammary, scapular, suprascapular, infra scapular and inter scapular regions.
Reduced breath sounds in left infrascapular region and left infra axillary region.
Reduced vocal resonance in the left sided infra axillary and infrascapular regions.
Provisional diagnosis: Based on the above history and examination, the most probable diagnosis is left sided pleural effusion, probably secondary to infection.
Investigations: total leukocyte count- 18000/cumm, hemoglobin- 14Gm/dL, platelets-2.89 lakhs/cumm


18100006009 THESIS
AUGUST 10, 2021
TITLE:
“EVALUATION OF CAROTID INTIMAL MEDIAL THICKNESS AND ESTIMATED GLOMERULAR FILTRATION RATE IN CHRONIC KIDNEY DISEASE”
INTRODUCTION:
Chronic kidney disease is characterized by a decrease in glomerular filtration rate and histological evidence of reduction in nephron population1.
The clinical course is typically one of a progressive loss of nephron function leading to end stage renal disease.
Kidney failure is the most common of the spectrum, but it represents only a minority of the total population affected by kidney disease.
The time between initial onset of disease and development of end stage renal failure may vary widely not only between different diseases with different histopathological findings but also in different patients with similar disease processes.
The progressive nature of CKD and the final stage ESRD is putting a substantial burden on global and national health resources since all modalities of treatment are expensive.
There are multiple causes of kidney injury that lead to the final common pathway of end stage renal disease, and this syndrome is characterized by hypertension, anaemia, nutritional impairment, neuropathy, renal bone disease, impaired quality of life, and reduced life expectancy.
Increasing evidence acquired in the past decades indicates that the adverse outcomes of CKD such as renal failure, cardiovascular disease, and premature death can be prevented or delayed by early detection of CKD3.
Earlier stages of CKD can be detected through laboratory testing only.
Treatment of earlier stages of chronic kidney disease, as well as initiation of treatment of cardiovascular and other risk factors at early stages of CKD should be effective in reducing the rate of progression of CKD to ESRD.
In patients with CKD, the atherosclerotic cardiovascular disease is leading cause for morbidity and mortality2.
Carotid intima-media thickness (CIMT) has been used as a marker for early atherosclerosis in patients.
The increased incidence of CVD is the consequence of a high prevalence of both traditional risk factors, uraemia-related, and “new factors,” such as infections (Herpes virus and Chlamydia pneumoniae) and hyper-homocysteinemia, oxidative stress, which increases atherosclerotic risk among these patients.
According to the 1999-2004 National Health and Nutrition Examination Survey (NHANES), the prevalence of Chronic Kidney Disease among the USA population is 15.3%.
It becomes apparent that the severity of CKD along with CVD severity in any population makes a very fatal combination for both patients and healthcare systems.
Approximately 50% of patients with ESRD die from a major cardiovascular event , which indicates a cardiovascular mortality that is 14 30times higher in dialysis patients and 500 times higher in 25- to 34- year-old ESRD patients than in individuals from the general population of the same age.
Studies have suggested that carotid intimal medical thickness can be used as a screening test as well as marker for atherosclerosis in cardio vascular disease.
Non-invasive assessment of intima medial thickness of carotid arteries by B – mode ultrasonography is used widely in observational studies and trials as an indicational measure of generalised atherosclerosis.
Increased intimal medial thickness of carotid arteries has been associated with disadvantageous levels of established cardiovascular risk factors, prevalent cardiovascular disease and atherosclerosis somewhere in the arterial system.
In this study the attempt to evaluate the association of increased intimal medial thickness with traditional and non-traditional cardiovascular risk factors in CKD patients was tried.
AIM:
Study of the carotid intimal medial thickness and estimated glomerular filtration rate in patients with Chronic Kidney Disease
OBJECTIVES:
Determine the stage of chronic kidney disease (CKD) depending on estimated glomerular filtration rate (eGFR)
To assess the carotid intimal medial thickness and estimated glomerular filtration rate in different stages of chronic kidney disease
To study the effect of cardiovascular risk factors on the grade of chronic kidney disease based on history and lipid profile of the patient.
To assess the carotid intimal medial thickness for detection of atherosclerosis in chronic kidney disease patients.
PATIENTS AND METHODS:
PLACE OF STUDY: The patients attending Internal medicine and nephrology department in Kamineni Institute of Medical Sciences, Narketpally.
STUDY DESIGN: Single centre, Cross sectional study
DURATION OF STUDY: 2 years (i.e. October 2018 to September 2020).
SAMPLE SIZE: 60 cases over 2 years
INCLUSION CRITERIA:
Patients diagnosed with chronic kidney disease getting treated at Department of Internal Medicine and Nephrology at Kamineni Institute of Medical Sciences, Narketpally.
EXCLUSION CRITERIA:
Patients with Nephrotic syndrome
Patients using statins
Patients on treatment with antiplatelets
Patients presenting with acute on chronic kidney disease
Patients with previous history of cardiovascular events
CONCLUSION AND SUMMARY:
High prevalence in traditional risk factors like diabetes, hypertension, smoking, age, alcohol, increased BMI was studied along with high prevalence in non-traditional risk factors like anaemia was studied.
More than half of the study population were illiterates
Less than 1/10th of patients showed positive family history
Carotid intimal medial thickness is a strong predictor of cardiovascular disease in CKD patients and maybe usefully applied in this group of patients
Association of carotid intimal medial thickness with diabetes mellitus in CKD patients is strong and maybe useful in this group of patients
Association of carotid intimal medial thickness with a non traditional risk factor like anaemia is strong as was correlated in this study
Association between carotid intimal medial thickness and dyslipidemia could not be established in this study
Association of carotiod intimal medial thickness with hypertension, smoking, alcoholism and obesity could not be correlated in this study
Identifying modifiable risk factors for the progression of cardiovascular disease may lead to targeted medical interventions in high-risk groups.
LINK TO COMPLETE THESIS WITH MASTER CHART
18100006009 LOG BOOK
AUGUST 10, 2021
I worked in kamineni institute of medical sciences as a post graduate in general medicine for 3 years. In this span I have to say that I saw the most interesting cases especially in the first half of my post graduation before covid.
A few cases I’ve found interesting are
1. A case of 24/M who had history of red coloured urine during night came with complaints of weakness, easy fatiguability and turned out to have paroxysmal nocturnal hemoglobinuria confirmed later on flow cytometry with minimal splenic vein thrombus covering about 30% of the lumen and is on followup
2. A 22/F came with history of chronic anemia turned out to be thalassemia trait with family history
3. A 21/F came with status asthmaticus (previous history of intubation and status asthmatic is present) and status epilepticus and was intubated for 7 days and was my first case that was extubated.
4. A case of 58/M with olanzapine induced dilated cardiomyopathy on maintainance haemodialysis well maintained over a year with only 1 hospitalisation history despite dialysis and heart failure
5. A case of 32/M with prosthetic valve and infective endocarditis of mitral valve
6. A 56/M with long standing diabetes mellitus with severe autonomic dysfunction presented with severe diabetic diarrhoea about 30 episodes of stools of normal consistency which responded to ondansetron after 5 days
7. A case of 16/F unmarried woman came with recurrent vomitings, raised liver parameters and turned out to self abort herself just before she got admitted in the hospital
8. A 30/M who came with community acquired pneumonia which was minimal on radiology and on examination on the first day with severe respiratory alkalosis turned out to involve the entire inferior sub pleural region of the right lung and had severe pleural pain
9. A 15/F came with recurrent diabetic ketoacidosis with poor control and increased food intake and got intubated twice in the same year
10. A 16/M with type 1 diabetes mellitus presented with green coloured urine, was suspected to have small intestinal bacterial overgrowth with vitamin b12 deficiency
11. A 24/M with vitamin e deficiency induced myelopathy which reduced over 6 months with treatment and followup
12. A 35/M who was referred from psychiatry for complaining of frequent change in colour of fingers during nights, turned out to have Raynaud’s phenomenon and had interstitial lung disease on examination was found to have systemic sclerosis on followup
13. A 25/F presented with severe shortness of breath and normal chest, heart findings, with respiratory alkalosis and metabolic acidosis turned out to have an exacerbation of systemic lupus erythematosis
14. A 18/M presented with complaints of acute pancreatitis without any history of alcoholism or prominent cause and turned out to have pancreas divisum on further investigations.
15. A 63/F with history of diabetes came with unilateral involvuntary movements was diagnosed to have diabetic chorea with hyper intensities on the caudate lobe.
16. A 42/F came with history of organophosphorus poisoning is a known case of left ventricular and septal aneurysm with descending thoracic aorta aneurysm, which might be worsened if given atropine as treatment for the poisoning.
17. A 18/F with nephrotic syndrome with focal segmental glomerulosclerosis on biopsy.
18. A 60/M came with post viral severe myocarditis and pericarditis with multiple episodes of paroxysmal atrial fibrillation? Secondary to chikungunya, learnt that cardiovascular involvement in chikungunya is the second most common system involved and is frequently under diagnosed.
Along with these few cases I’ve seen while working here, some interesting cases I’ve seen in my peripheral postings are
1. A large cardiac thrombus in the left ventricle in an asymptomatic patient
2. A case of severe pulmonary artery hypertension with multiple valvular abnormalities
3. A diagnosed case of wegeners granulomatosis in end stage renal failure
4. A patient with bmi- 46 and metabolic syndrome on end stage renal failure
If I have to say that I learnt a procedure well, I would have to say that I developed a special interest in cardiology while working here and went to the 2d echo machine everyday in the evening with a patient and started to learn on normal hearts first. Overtime I started seeing abnormalities by myself which was overwhelming to me.
I gained a lot of experience dealing with multiple acute kidney injuries, chronic kidney disease cases with the exposure any nephrology post graduate would have normally and gained confidence in managing an emergency patient with renal failure.
I gained a lot of experience in placing central venous catheters, right jugular, left jugular and femoral catheters. I placed atleast 73 catheters during my nephrology peripheral postings.
HALL TICKET 18100006010
CASE PRESENTATIONS
AUGUST 10, 2021
LONG CASE:
A 45 year old male, daily wage labourer came to the casualty with
CHIEF COMPLAINTS:
Imbalance while walking since 3 days associated with Swaying to both the sides since 3 days. Involuntary movements of the extremities since 3 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 3 days back then in the morning after he had his breakfast he noticed *imbalance while walking along with swaying on both the sides which was sudden in onset, progressive in nature, associated with generalized weakness and falls without loss of consciousness. *Involuntary movements of the extremities particularly upper limbs since 3 days, symmetrical, which was aggravating while trying to reach an object and relieving with rest, interrupting with his daily activity.
No history of buckling of limbs
No history of stiffness of limbs
No history of difficulty in getting up from squatting position
No history of any difficulty in rolling over the bed.
No history of otorrhea or any hearing loss or any earache.
No history of giddiness or lightheadedness or palpitations, dry skin
No history suggestive of wash basin attack
No history of difficulty in wearing slippers or any slippage of chappals.
No history of any root pain or paresthesias or numbness
No history of neck pain or neck stiffness or blurring of vision or projectile vomitings.
No history of urinary incontinence or retention or diarrhea or constipation.
No history of any speech abnormality or anything suggestive of cranial nerve abnormality.
No history of fever or headache
No history of waxing or wanning of symptoms.
No history of any behavioural changes
No history of weight loss or loss of appetite.
No history of intake of toxins.
No history of joint pains or rash
No history of bulky stools or loose stools.
PAST HISTORY:
Known case of epilepsy and on medication since 8 yrs (Tab PHENYTOIN 100MG/TID)
Not a known case of diabetes or hypertension or thyroid problems or tuberculosis.
No history of any serious illness in the past or any hospital admission
No history of similar complaints in the past.
DRUG HISTORY:
History of excessive intake of phenytoin in the past 20 days for the fear of precipitating seizures.
PERSONAL HISTORY:
Regular diet
Regular bowel and bladder
Disturbed sleep since past 1 month (due to anxiety and depression probably due to loss of
his brother) Occasionally Alcoholic. Occasional Smoker: smokes 1 pack (20 cigarretes) in a week ,0.5 pack years
FAMILY HISTORY:
Born on non consanguinous marraige.
achieved appropriate developmental milestones.
No history of similar complaints in the family.
SUMMARY:Case of a 45 Year old male with symmetrical bilateral Ataxia, sudden in onset,
I would like to consider the possibility of Acute cerebellar Ataxia without the involvement
of sensory, motor, autonomic or cranial nerve involvement.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative, comfortably lying on bed.
Well built, moderately nourished, BMI of 22kg/m2.
No pallor/ icterus /cyanosis/clubbing/ kylonychia /lymphadenopathy/edema
Hypertrophy of the gums present.
No signs of Neurocutaneous markers or any skin rash
No hyperpigmentation of knuckles.
No signs of nutritional deficiency like cheilitis or angula stomatitis or purpura or thinning of hair or dermatitis or bruising.
No spine abnormalities
No signs of skeletal deformities like pes cavus , short neck.
No detectable KF rings or sunflower cataract or telangiectasias.
VITALS:
PULSE: regular rhythm
82 BPM
good volume
normal character
normal vessel wall thickening
no radioradial or radiofemoral delay.
peripheral pulses felt.
BLOOD PRESSURE: right arm supine position.
132/90mm of hg
RESPIRATORY RATE: 22CPM, regular, abdominothoracic type.
TEMPERATURE : afebrile
SYSTEMIC EXAMINATION:
CNS:
Right Handed person, studied upto 10th standard.
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
MMSE 26/30
speech: normal
Behavior: normal
Memory: Intact.
Intelligence: Normal
Lobar Functions: Normal.
No hallucinations or delusions.
CRANIAL NERVE EXAMINATION:
1st : Normal
2nd : visual acuity is normal
visual field is normal
colour vision normal
fundal glow present.
3rd,4th,6th : pupillary reflexes present.
EOM full range of motion present
gaze evoked Nystagmus present.
5th : sensory intact
motor intact
7th : normal
8th : No abnormality noted.
9th,10th : palatal movements present and equal.
11th,12th : normal.
MOTOR EXAMINATION: Right Left
UL LL UL LL
BULK Normal Normal Normal Normal
TONE hypotonia hypotonia hypotonia hypotonia
POWER 5/5 5/5 5/5 5/5
SUPERFICIAL REFLEXES:
CORNEAL present present
CONJUNCTIVAL present present
ABDOMINAL present
PLANTAR withdrawal withdrawal
DEEP TENDON REFLEXES:
BICEPS 2 2 2 2
TRICEPS 2 2 2 2
SUPINATOR 2 2 2 2
KNEE 2 2 2 2
ANKLE 1 1 1 1
SENSORY EXAMINATION:
SPINOTHALAMIC SENSATION:
Crude touch
Pain
Temperature
DORSAL COLUMN SENSATION:
Fine touch
Vibration
Proprioception
CORTICAL SENSATION:
Two point discrimination
Tactile localisation.
Steregnosis
Graphasthesia.
CEREBELLAR EXAMINATION:
Finger nose test
Heel knee test
Dysdiadochokinesia
Dysmetria
Hypotonia with pendular knee jerk present.
Intention tremor present.
Rebound phenomenon.
Nystagmus
Titubation
Speech
Rhombergs test
SIGNS OF MENINGEAL IRRITATION: absent
GAIT:
Wide based with reeling while walking, unsteady with a tendency to fall
unable to perform tandem walking.
CVS EXAMINATION:
S1 S2 Present
No murmurs or added sounds
RESPIRATORY SYSTEM EXAMINATION:
Bilateral airway entry
No added sounds.
PER ABDOMEN EXAMINATION:
Soft and nontender.
No organomegaly present.
FINAL DIAGNOSIS:
FUNCTIONAL: ATAXIA
ANATOMICAL: CEREBELLUM
PATHOLOGICAL:
ETIOLOGICAL: ? DRUG INDUCED(PHENYTOIN)
WORKUP:
CBP:
HB 11.2
TLC 12000
PLATELET 2.02L
ESR 23
LFT Within normal limit
RFT Within normal limit
ECG
CXRAY
-------------------------------------------------------------------------------------------------
SHORT CASE-1:
A 60 years old female presented to the casualty with complaints of fever associated with chills and abdominal pain.
CHIEF COMPLAINTs
➤Fever for the past 6 days.
➤Pain abdomen for the past 3 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 6 days ago after which she developed high grade fever associated with chills, insidious in onset, progressive, not subsiding with medication, continuous type
Pain abdomen, sudden in onset, pricking type, in the epigastrium and right hypochondrium which gets aggravated on right lateral position and relieved with sitting posture, associated with nausea and reduced appetite, no association with intake of fatty food
No complaints of burning micturition.
No complaints of cough, cold or shortness of breath.
No complaints of heartburn or flatulence.
No complaints of heamatemesis or maleana.
No complaints of dysphagia.
No complaints of constipation or diarrhoea.
No history of yellowish discolouration of eyes or high coloured urine.
No history of weight loss
No history of any blood transfusion
No history of any high risk behaviour
HISTORY OF PAST ILLNESS
Not a known case of hypertension, diabetes, bronchial asthma, epilepsy.
k/c/o tuberculosis and took complete treatment.
No history of similar complaints in the past.
DRUG HISTORY
➤No significant drug history or intake of toxins.
PERSONAL HISTORY
➤Occupation: Daily waged labor working in Cotton fields.
➤Patient is married
➤Patient takes mixed diet but has a decreased appetite.
➤Bowel and bladder movement is normal and regular.
➤occasional Alcoholic, non smoker.
- sound sleep
FAMILY HISTORY
➤No significant family history.
MENSTRUAL HISTORY:
G 3 P 4 L 4 A 0
Attained menarche at the age of 20 years, with good flow and volume.
Attained menopause at age of 42 years.
SUMMARY:
60 year old female with high grade fever and abdominal pain confined to
right upper quadrant, acute in onset, without any alcohol history.
Possibly case of
1) Acute Liver injury (?infective etiology)
2)Acute Cholecystitis.
GENERAL EXAMINATION
Patient is well built, well nourished.
➤Pallor: Not seen
➤Icterus: Not seen
➤Cyanosis: Not seen
➤Clubbing: Not seen
➤Lymphadenopathy: Not seen
➤Edema: Not seen
- No signs of chronic liver cell failure
- No signs of nutritional deficiency.
VITALS
➤Temperature: 101℉
➤PR: 108 beats per minute
➤BP: 100/70 mmHg
➤RR: 24 cycles per minute
➤SpO2: 95% in room air
➤Blood Sugar (random): 100mg/dl
SYSTEMIC EXAMINATION
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid, with no distention.
➤Umbilicus - Inverted
➤Equal symmetrical movements in all the quadrants with respiration.
➤No visible pulsation,peristalsis, dilated veins and localized swellings.
PALPATION
➤SUPERICIAL: Local rise of temperature in right hypochondrium with tenderness
and localised guarding and rigidity.
➤ DEEP: Mild enlargement of liver, regular smooth surface, rounded
edges soft in consistency, tender, moving with
respiration non pulsatile
➤No splenomegaly
➤Abdominal girth: 78cms.
➤xiphesternum to umbilicus distance was equal to umbilicus to pubic distance.
PERCUSSION
➤Hepatomegaly: liver span of 16 cms with 4 cms extending
below the costal margin
➤Fluid thrill and shifting dullness absent
➤Puddle sign absent
➤Traubes space: resonant
AUSCULTATION
➤ Bowel sounds present.
➤No bruit or venous hum.
NO LOCAL LYMPHADENOPATHY
PER VAGINAL AND PER RECTAL EXAMINATION: NAD
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
PROVISIONAL DIAGNOSIS:
ACUTE HEPATITIS (? INFECTIVE)
INVESTIGATIONS:
DAY 1
Serum Na+ 126
Serum K+ 4.7
Serum Cl- 92
Serum Creatinine 0.8
Blood urea 40
CUE normal
CBP: HB 10.7
TLC 13900
PLATELET 4.02L
LFT: TB 2.45
DB 1.59
SGOT 52
SGPT 10
ALK P 191
ALB 2.5
PT/INR 17/1.2
APTT 33SECS
ESR 110
BLOOD CULTURES Showed no growth.
USG ABDOMEN
 |
USG REPORT IMPRESSION- Multiple liver abscess with largest measuring 5*5 cms in the 7th segment of liver , with 40 to 50% of liquefaction , hepatomegaly with liver span of 18.5 cms.
CT SCAN


|
 |
XRAY CHEST-POST TB CHANGES
|
FINAL DIAGNOSIS :
MULTPLE PYOGENIC LIVER ABSCESS WITH ACUTE LIVER FAILURE.
TPR CHART
-------------------------------------------------------------------------------------------------
SHORT CASE-2:
A 48 yr old male, farmer by occupation & resident of Nakrekal came to casualty with
CHEIF COMPLAINTS:
1.Swelling in the right lower limb since 20 years
associated with pain
2.Fever since 1wk
3.Loose stools since 4 days (4 episodes/day)
HISTORY OF PRESENT ILLNESS :
Patient was apparently asymptomatic 20years back then, he developed
1) SWELLING IN THE RIGHT LOWER LIMB:
-Patient is a known case of filariasis with right leg swelling since 20 years which gets aggravated with rest and subsided with walking intermittently also associated with fever spikes which gets relieved with medication
- Patient had a trauma over right lower limb 4 days back, following which patient noticed increased swelling over right leg with ulceration and pus discharge associated with pain of pricking type.
2) FEVER:
- Low grade, intermittent type, associated with chills & rigors, since 1 week & relieved by medications.
- He got admitted for the same in a nearby hospital and was told that
his platelet count is low for which he was receiving conservative
treatment, as he could'nt afford the charges so was shifted here.
3)LOOSE MOTIONS:
-Patient had loose motions since 4 days, upto 4 episodes per day,
not blood stained, non mucoid, low volume, non foul smelling.
No history of body pains, abdominal pain, headache.
No history of nausea ,vomitings or diarrheoa.
No history of oliguria or burning micturition.
PAST HISTORY:
- No similar complaints in the past
-Not a k/c/o DM, HTN, Asthma, TB, Epilepsy.
-No history of any drug usage or intake of toxins.
FAMILY HISTORY -
-No significant family history
PERSONAL HISTORY-
- Diet :mixed
- Appetite :normal
- Sleep : adequate
- Bladder : regular.
- Bowel : diarrheoa since 4 days.
- Addictions : Absent
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative.
well built, moderately nourished.
- No pallor
- No icterus
- No clubbing, cyanosis
- No koilonychia
- No lymphadenopathy
- No Edema
- No rashes, Petechiae & Bleeding manifestations
-Tourniquet test - Negative
VITALS:
1.Temperature: Afebrile
2. BP : 100/70mmHg
3. PR : 74 bpm
4. RR : 24cpm.
SYSTEMIC EXAMINATION:
PER ABDOMEN:
- No distended abdomen
- No abdominal tenderness
- No engorged veins
- Guarding & rigidity absent
- Bowel sounds present.
RESPIRATORY SYSTEM:
-Bilateral airway entry present
-No added sounds
CVS:
- S1S2 Heard
- No thrills no murmurs
CNS:
-No abnormality noted
- Higher mental functions intact.
LOCAL EXAMINATION:
PROVISIONAL DIAGNOSIS:
-ELEPHENTIASIS WITH CHRONIC LYMPHEDEMA
-DENGUE FEVER
FEVER CHARTING:
SURGERY REFERRAL:
INVESTIGATIONS:
HEMOGRAM:
DATE: 4/08/21
- TOTAL WBC COUNT - 5,250 cells/cumm (N - 4,000 to 10,000 cells/cumm)
- PLATELET COUNT - 1.99 lakhs/cumm (N - 1.5 - 4.1 lakh/cumm)
- PCV - 38.3% (N - 40 - 50 %)
- 6/08/21
- TOTAL WBC COUNT - 3,500 cells/cumm
- PLATELET COUNT - 1.25 lakhs/cumm
- PCV - 46%
- 7/08/21
TOTAL WBC COUNT - 2,150 cells/cumm
- PLATELET COUNT - 44,000 cells/cumm
- PCV - 39%
- 8/08/21 (MORNING)
- TOTAL WBC COUNT - 3,650 cells/cumm
- PLATELET COUNT - 39,000 cells/cumm
- PCV - 39.4%
- 8/08/21 (EVENING)
- TOTAL WBC COUNT - 4,200 cells/cumm
- PLATELET COUNT - 60,000 lakhs/cumm
- PCV - 39.1%
- 9/08/21 (Morning)
Evening
DENGUE RAPID TEST
MALARIAL PARASITE TEST
LFT
CUE
RBS
BLOOD UREA
SERUM CREATININE
SERUM ELECTROLYTES
ECG
TREATMENT
DATE - 08/08/21
1. IVF @ 75 Ml/hr
- 1. NS
- 1. RL
- 1. DNS
2. TAB PCM 650 MG X PO X TID
1 - 1 - 1
Check temperature before giving pcm
3. TEMPERATURE CHARTING 4TH HRLY
4. GRBS CHARTING 6TH HRLY
5. I/O CHARTING
DATE - 9/09/21
1. IVF @ 75 Ml/hr
- 1. NS
- 1. RL
- 1. DNS
2. TAB PCM 650 MG X PO X TID
1 - 1 - 1
3. TAB AUGMENTIN 625 MG X OD X BD
4. TAB PAN 40 MG X OD
5. TAB MVT ORAL OD
6. TAB VIT C ORAL OD
7. TAB DOLO 650 MG ORAL (SOS)
8. Check temperature before giving pcm
9. TEMPERATURE CHARTING 4TH HRLY
10.GRBS CHARTING 6TH HRLY
11. I/O CHARTING
18100006010 THESIS
AUGUST 10, 2021
TITLE:
SIGNIFICANCE OF SERUM PSEUDOCHOLINESTERASE LEVELS IN PATIENTS WITH ORGANOPHOSPHORUS COMPOUND POISONING”
INTRODUCTION:
Acute poisoning is important cause of morbidity and mortality in India. In medical emergency 10% of admissions are due to poisoning and organophosphorus poisoning contributes to nearly 50% of it.[1] Apart from use of these substances as agricultural insecticides, pesticides, they are frequently abused for suicidal purposes because of their low cost, rapid action and easy availability. They have been imported in India since 1951, but very few knew the nature of these compounds as a virulent poison till the Kerala food poisoning tragedy in 1958. This tragedy took a toll of hundred and add due to inadvertent stocking of food stuff and folidol packages in the same hold where the folidol containers leaked and contaminated the gunny bags containing food stuff [2]. Exposure to organophosphorus compounds in the form of nerve agents and pesticides poses an ever increasing military and civilian threat [3] the majority of patients are younger than 30 yrs. [5] In teenagers and adults the poisoning is generally due to suicidal intention though accidental poisoning occurs during spraying [2] They act by irreversibly inhibiting the enzyme cholinesterase resulting in accumulation of acetylcholine at synapses and myoneural junction and leads to cholinergic over activity.[6][7][8]
AIMS AND OBJECTIVES
AIM:
To study the significance of serum pseudocholinesterase levels in patients with organophosphorus compound poisoning.
OBJECTIVES:
To study the clinical manifestations in patients with organophosphorus compound poisoning
To study the prognostic and diagnostic value of serum pseudocholinesterase levels in patients with organophosphorus compound poisoning.
To study the outcome of patients with organophosphorus compound poisoning.
MATERIALS AND METHODS:
SOURCE DATA:
This study was undertaken from October 2018 to September 2020 at Kamineni Institute of Medical Sciences, Narketpally.100 patients of suspected organophosphorous poisoning admitted to medical emergency ward, Kamineni Institute of Medical Sciences have formed the material for the study.
STUDY DESIGN:
Single centre
Prospective study
INCLUSION CRITERIA:
In this study patients above 18 years with suspected Organophosphorus compound poisoning
EXCLUSION CRITERIA:
• OP compound poisoning cases < 18 years of age.
• H/o consumption of other drugs along with OP compound
• H/o preexisting hepatic dysfunction which reduce the level of Pseudocholinesterase.
• History of Carbamate poisoning.
DIAGNOSIS:
Based on
1) History or evidence of exposure to organophosphorus compound within 24hours.
2) Characteristic manifestations of OPC poisoning including, miosis,
fasciculations, excessive salivation.
3) Improvement of signs and symptoms with administration of atropine.
4) Corroborative evidence like empty containers and odour of gastric aspirates.
Depending on the severity of manifestations patients were classified into three grades as mild, moderate and severe depending on serum pseudocholinesterase levels.
INVESTIGATIONS:
Soon after admission blood samples were collected and investigated to know the serum levels of pseudocholinesterase on Day 1, Day 3, and before discharge. Other routine investigations such as
• Hemoglobin percentage
• Total blood count
• Differential count
• ESR
• Random blood sugar
• Serum creatinine
were done to exclude chronic conditions.
METHOD OF ESTIMATION OF PSEUDOCHOLINESTERASE:
Method with S-butyryl thiocholine iodide using Dibucaine as inhibitor.
LINK TO COMPLETE THESIS WITH MASTER CHART:
18100006010 LOG BOOK
AUGUST 10, 2021
I feel very fortunate for practicing the branch of my choice where I get to see vast variety of cases on day-to-day basis. Here I will be sharing few of my experiences during my junior residency.
I have seen closely majority of cases during my first year of residency. One of the mind blowing case was of Non Hodgkins Lymphoma:
Patient presented with fever of high grade with anorexia, he was almost worked up for 2 weeks but we couldnt find any conclusive diagnosis. we ultimately labelled him as pyrexia of unknown origin. Then gradually after weeks of stay in hospital patient started developing vague abdominal pain which made us repeat his USG abdomen and Erect X ray abdomen which showed mediastinal lymphadenopathy.
we tried palpating the rest group of lymph nodes for any enlargement but there was only mediastinal lymphadenopathy, as we couldn't get any cause for his lymph node enlargement, we planned for a lymph node biopsy CT guided, which showed features suggestive of non Hodgkins lymphoma.